The Digestive System Anatomy
The Digestive System Laboratory Activity
The digestive system is made up of a series of hollow organs that form a tube that twists and convolutes (~30 meters long) and the main functions are to convert food into fuel.
Food enters the digestive tract at the mouth where digestion begins and continues along the digestive tract, processes such as absorption and production of waste also happen here. The digestive system contains accessory organs such as the liver, gallbladder and pancreas that help break down and absorb food.
The organs that make up the digestive tract are: the mouth (oral cavity), esophagus, stomach, and small intestine (duodenum, jejunum, and ileum), large intestine (colon, rectum, and anus). These hollow organs are composed of several layer of tissue, the mucosa contains glands that produce substances to help digest food and lubricate (lines the lumen), sub mucosa, the smooth muscle layer (middle layer) helps break down food and move it along the tract and a serosa layer, protective connective tissue layer (adventitia).
The liver and the pancreas produce digestive secretions that reach the intestine through small tubes called ducts. The gallbladder stores the bile (produced in the liver) until needed in the intestine. Parts of the nervous (plexuses) and circulatory systems play major roles in the digestive system.
Let’s examine the structure and function of each of the organs that form the digestive system.
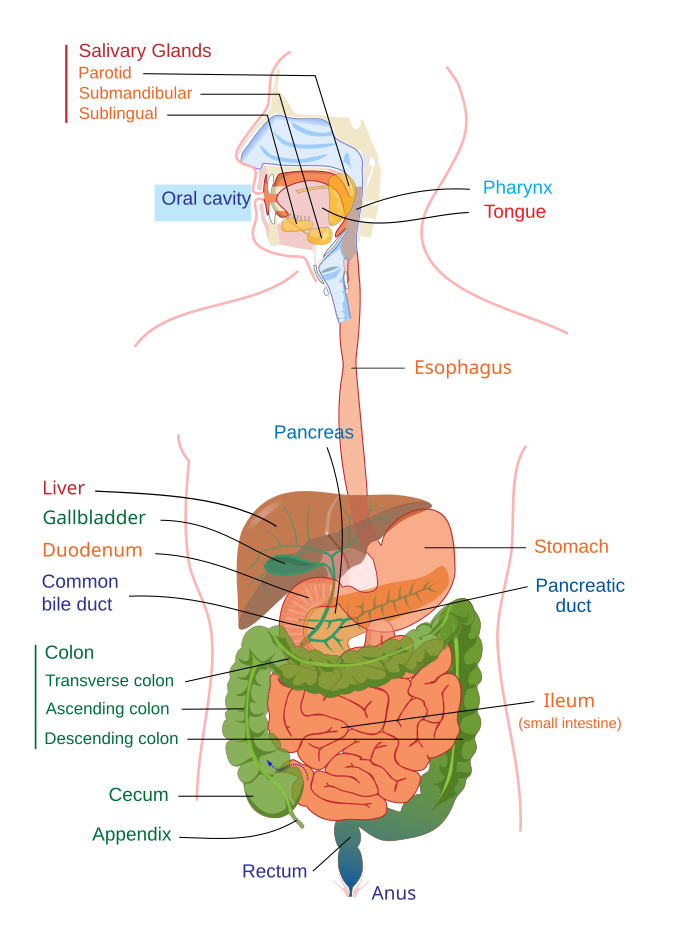
The Digestive System
Mouth (Oral Cavity)
Movement: Mastication
Secretions (Fluid/Enzymes/Hormones/Mucus)
- Saliva (H2O, HCO3-)
- R-protein (protection of B-12)
- Salivary amylase (ptyalin = α-amylase) to maltose, maltriose
- *Greek ptyalon saliva, from ptyein to spit
- Serous Mucus (lubrication), helps soften the food and form it into a bolus.
- Lingual lipase, hydrolyzes long-chain triglycerides into partial glycerides and free fatty acids.
Digestion: Beginning carbohydrate and lipid breakdown
Absorption: Very little
Reflexes: Chewing or Mastication Reflexes
Innervation:
- Cranial nerves
- Sympathetic
- Parasympathetic
Disorders
- Cleft lip/palate
- Dental decal
- Tooth loss
- Tone damage
- TMJ
- Paralysis/ spinal cord injury
- Sjorngren’s syndrome🡪inability to produce saliva or tears
Teeth
- Primary teeth are the first set of teeth that erupt through the gums at regular intervals between the ages of six months and two and one-half years. There are twenty primary teeth – ten in each jaw.
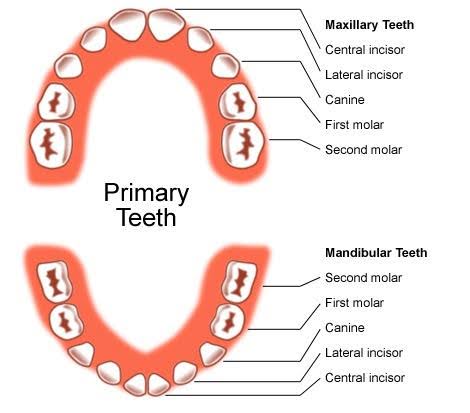
- Secondary teeth begin to appear about age six but may not be completed until age twenty-five.
- There are thirty-two secondary teeth – sixteen in each jaw.
- The incisors are chisel-shaped, and their sharp edges bite off relatively large pieces of food.
- The cuspids (canine) are cone-shaped, and they grasp and tear food.
- The bicuspids (premolars) and molars have somewhat flattened surfaces and are specialized for grinding food particles.
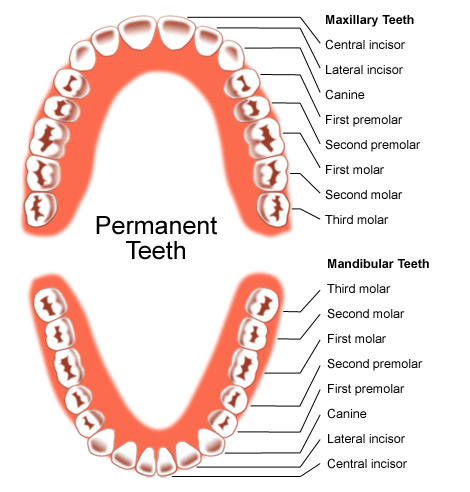
Permanent Teeth
Each tooth consists of two main portions called the crown and the root. The crown is the portion above the gum and is covered by glossy white enamel. Beneath the enamel is the bulk of the tooth, which is made up of dentin. Dentin surrounds the central cavity, which houses the blood vessels, nerves and connective tissue. The root is enclosed by cementum, which is surrounded by the periodontal ligament. The region where the crown and root meet is called the neck. The cementum and the periodontal ligaments anchor the tooth to the alveolar bone.
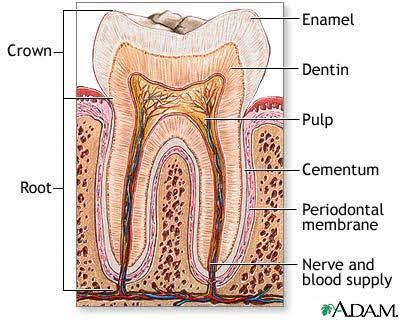
The Histological Structure of a Tooth
Pharynx
The pharynx is the part of the neck and throat situated behind the mouth and nasal cavity, and cranial, or superior, to the esophagus.
It is part of the digestive system and respiratory system. Because both food and air pass through the pharynx, a flap of connective tissue, the epiglottis closes over the trachea when food is swallowed to prevent choking or asphyxiation.
The pharynx is composed of:
The nasopharynx located above the soft palate, lies behind the nasal cavity and like the nasal passages is lined with ciliated columnar pseudostratified epithelium.
The oropharynx located behind the soft palate and projects downward to the upper border of the epiglottis, is that part of the pharynx behind the oral cavity. It is lined with stratified squamous epithelium.
The laryngopharynx (hypopharynx) located from the upper border of the epiglottis downward to the lower border of the cricoid cartilage of the larynx, where the respiratory and digestive pathways diverge. At that point, the laryngopharynx is continuous with the esophagus. It serves as a passageway for food and air, during swallowing, food has the “right of way”, and air passage temporarily stops. It is lined with a stratified squamous epithelium.
Swallowing
The steps in the mechanism of swallowing are:
- The soft palate rises, preventing food from entering the nasal cavity.
- The hyoid bone and the larynx are elevated; the epiglottis closes off the top of the trachea so that food is less likely to enter.
- The tongue is pressed against the soft palate, sealing off the oral cavity from the pharynx.
- The longitudinal muscles in the pharyngeal wall contract, pulling the pharynx upward toward the food.
- The lower portion of the inferior constrictor muscles relaxes, opening the esophagus.
- The superior constrictor muscles contract, stimulating a peristaltic wave to begin in the pharyngeal muscles. This wave forces the food into the esophagus.
Esophagus
The esophagus is a narrow and hollow muscular tube about 20-30 centimeters long, closed proximally and distally by muscular sphincters.
The esophagus functions as a tube that transports substances from the pharynx to the stomach.
The upper esophageal sphincter (UES) and proximal one third of the esophageal body is composed of striated muscle. There is then a transition zone where striated and smooth muscles intermix. The lower esophageal sphincter (LES) and the distal one half to two thirds of the esophageal body are composed of smooth muscle
The esophageal wall is composed of distinct layers:
- The inner mucosal layer consists of stratified squamous epithelium and underlying connective tissue, within which lies a longitudinally oriented muscle layer called the muscularis mucosa (unknown function)
- The muscularis propria, involved in bolus transport and consists of an inner layer of circularly oriented muscle fibers and an outer layer of longitudinally oriented fibers.
- In between these two muscle layers lies the myenteric plexus, which controls the motor function of these muscles.
The main function of the esophagus is to propel swallowed food or fluid into the stomach.
The peristaltic velocity averages about 3 cm/sec in the upper esophagus, then accelerates to about 5 cm/sec in the mid-esophagus, and slows again to approximately 2.5 cm/sec distally.
The duration and amplitude of individual pressure waves also varies along the esophagus. The duration of the wave is shortest in the proximal esophagus (approximately 2 seconds) and longest distally (approximately 5 to 7 seconds). In average, it takes about seven seconds for food to pass through the esophagus.
Movements:
- Peristalsis: rhythmic propelling movements that occur in the alimentary canal
- Receptive relaxation is where the muscular wall ahead of peristaltic contraction relaxes. This allows the tubular contents to be pushed along the canal.
- Secretions (Fluid/Enzymes/Hormones/Mucus): Lubricating Mucus
- Digestion: Starch continued from above
- Absorption: None
- Reflexes: Receptive relaxation
- Innervation: Cranial nerves, Parasympathetic, Sympathetic
Disorders:
- Achalasia—lower esophageal sphincter fails to relax during the swallowing mechanism—damage to lower 2/3 of the esophagus, may lead to megaesophagus—excessive distension of the esophagus; heartburn (GERD); esophagitis (inflammation of the esophagus); paralysis; hernia, diverticula, and atresia
Stomach
The stomach is a J-shaped, pouch-like organ. Thick folds called rugae mark its inner lining. Its mucous membrane lining contains the gastric pits that are the openings for the gastric glands that secrete digestive enzymes.
Movement: Peristalsis, Retropropulsion/ mixing
Secretions (Fluid/Enzymes/Hormones/Mucus):
- Gastric fluid, intrinsic factor, and HCl/Pepsin, Tributerase, and collagenase/Gastrin and Histamine/thick, viscous, basic mucous.
- Chief cell-Pepsinogen
- Parietal cell-HCl (convert pepsinogen to pepsin) and intrinsic factor (for absorption of B-12)
- Neck cell-Mucus (protection)
- Surface epithelial cell- Bicarbonate (protects mucosa)
- Mucosal cells- Histamine (↑ acid production)
- G-cells- Gastrin (↑ acid production, ↑ intestinal motility, pyloric contraction, ↑ secretion of Secretin, and relax ileocecal valve)
- Pepsin—is a protein-splitting enzyme. The chief cells secrete pepsinogen (the precursor of pepsin) that then combines with hydrochloric acid to form pepsin.
- Intrinsic factor—aids in the absorption of vitamin B12
Digestion:
- Starch continued from above until pH reaches ~4.
- Beginning of protein breakdown to proteases, peptones, and poly-peptides by pepsin.
- Absorption: Some lipid-soluble substances such as alcohol (20%) and aspirin.
Reflexes:
- Regulation of gastric secretions
- Parasympathetic impulses and the hormone gastrin enhance the gastric secretions. The presence of the food in the small intestine🡪 inhibits the gastric secretions.
Mechanism that controls the emptying of the stomach.
The chyme accumulates near the pyloric sphincter. This muscle begins to relax. The pyloric region of the stomach then pumps the chyme a little at a time into the small intestine. The rate at which the stomach empties is dependent upon the fluidity of the chyme and the type of food present.
- Gastrocholic reflex—signals from the stomach cause evacuation of the colon.
- Enterogastric reflex— inhibits the gastric peristalsis and secretion when the food enters the small intestine. The small intestine tells the stomach to slow down (negative feedback).
Innervation: Vagal nerves (Parasympathetic) Sympathetic
Disorders
Peptic ulcer disease (PUD) gastric ulcers in the stomach
- Gastritis— inflammation of the gastric mucosa,
- Gastric atrophy—in people with chronic gastritis, the mucosa becomes atrophic until little or no gastric gland activity remains.
Autoimmunity, may lead to:
- Achlorhydria—no HCl secretion, [can be due to chronic use of antacids, no carbonic anhydrase].
- Hypochlorhydria—diminished HCl secretion,
- Pernicious anemia-no intrinsic factor (B-12 absorption problem)🡪 failure to synthesize RBC’s
Hiatal Hernia
Pyloric stenosis (esp. in children)
Small intestine
is the part of the gastrointestinal tract following the stomach and followed by the large intestine, and is where much of the digestion and absorption of food takes place. It receives bile juice and pancreatic juice through hepato-pancreatic duct, controlled by Sphincter of Oddi
The primary function of the small intestine is the absorption of nutrients and minerals found in food.
The average length of the small intestine in an adult human male is 6.9 m (22 feet 6 inches), and in an adult female 7.1 m (23 feet 4 inches). It can vary greatly, from as short as 4.6 m (15 feet) to as long as 9.8 m (32 feet). It is approximately 2.5–3 cm in diameter.
The small intestine is divided into three structural parts:
- Duodenum—the first twenty-five centimeters of the small intestine, it lies behind the parietal peritoneum. It is the most fixed portion of the small intestine.
- Jejunum—the proximal two-fifths of the remainder of the small intestine.
- Ileum—the remainder of the small intestine
The three sections of the small intestine look similar to each other at a microscopic level, but there are some important differences. The parts of the intestine are as follows:
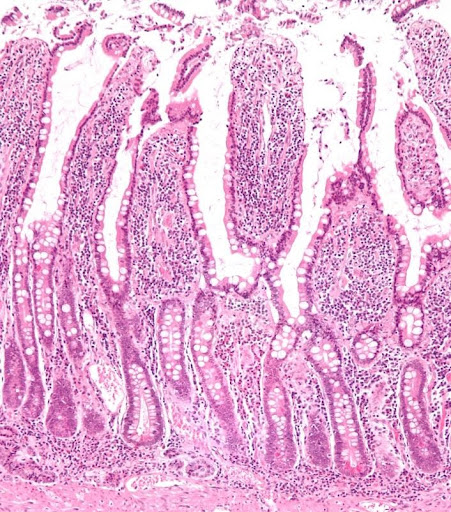
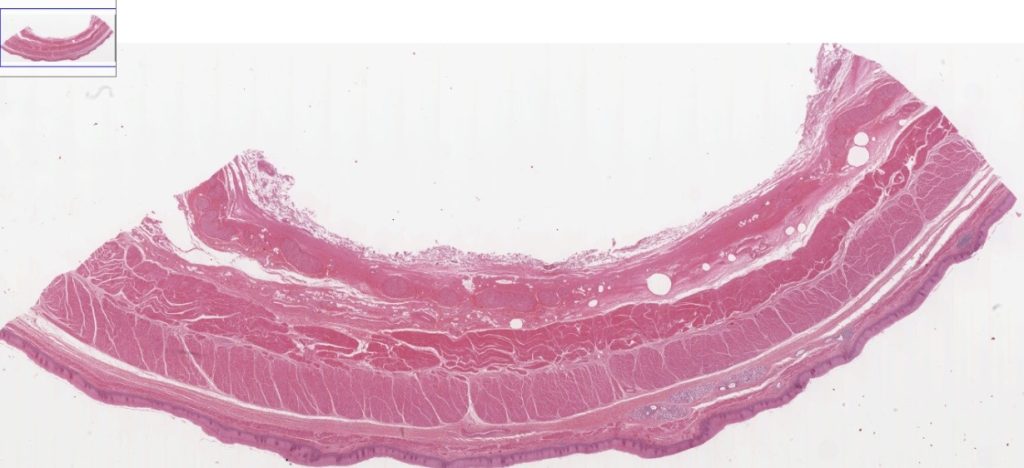
Histology
The small intestine is divided into duodenum (25-30 cm), jejunum (about first two-fifths of the rest) and ileum. The three segments merge imperceptibly and have the same basic histological organization.
The Mucosa
The mucosa of the small intestine has various structural features which considerably increase the luminal surface area and consequently support the main function of the small intestine – the absorption of the degraded components of the food.
Plicae circulares (of Kerkering) are macroscopically visible, crescent-shaped folds of the mucosa and submucosa. Plicae circulares extend around one-half to two-thirds of the circumference of the lumen of the small intestine.
Plicae circulares
- Are permanent structures, i.e. their presence does not depend on the state of distension of the small intestine.
- Are absent from the first few centimeters of the duodenum and the distal part of the ileum.
- Are particularly well developed in the jejunum.
- Increase the surface area of the mucosa by a factor of ~ three.
The entire intestinal mucosa forms intestinal villi (about one mm long), which increase the surface area by a factor of ~ ten. The surface of the villi is formed by a simple columnar epithelium. Each absorptive cell or enterocyte of the epithelium forms numerous microvilli (1 µm long and about 0.1 µm wide). Microvilli increase the surface area by a factor of ~ 20.
Between the intestinal villi we see the openings of simple tubular glands, the crypts of Lieberkühn. They extend through the lamina propria down to the muscularis mucosae. Undifferentiated cells close to the bottom of the crypts regenerate the epithelium (epithelial cell turnover time is less than one week). Other epithelial cells in the crypts correspond largely to those in the epithelium of the intestinal villi. One exception is Paneth cells, which are located at the bottom of the crypts. They release a number of antibacterial substances, among them lysozyme, and are thought to be involved in the control of infections.
One function of the crypts of Lieberkühn is the secretion of “intestinal juice” (about 2 liter/day), which in its composition closely resembles extracellular fluid and which is rapidly reabsorbed. The only enzymes which can be demonstrated in the intestinal juice are enteropeptidase (or enterokinase), which activates the pancreatic enzyme trypsin, and small amounts of amylase. In addition to enterocytes, the epithelium is composed of mucus-secreting goblet cells and endocrine cells.
In addition to gastrin- and somatostatin-producing cells, we also find endocrine cells secreting cholecystokinin and secretin. Cholecystokinin stimulates the secretion of digestive enzymes in the pancreas and the contraction of the gall bladder. Secretin stimulates the pancreas to release “pancreatic juice”, which is rich in bicarbonate ions. Secretin also amplifies the effects of cholecystokinin.
The lamina propria is, similar to the lamina propria of the stomach, unusually cell rich. Lymphocytes often invade the epithelium or form solitary lymphoid nodules in the lamina propria. Lymph nodules may form longitudinal aggregations of 30-50 nodules in the lamina propria of the ileum. These large aggregations are called Peyer’s patches.
The muscularis mucosae has two layers and extends into the intestinal villi, where the smooth muscle cells form a longitudinal bundle in the center of the villi.
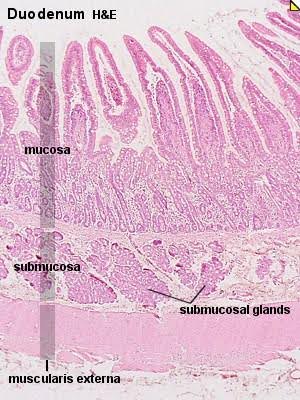
The Submucosa
The submucosa contains glands only in the duodenum. Submucosal glands of the duodenum are also called Brunner’s glands. Their secretion is mucous and slightly alkaline due to bicarbonate ions (pH 7-8). The amount of bicarbonate is however too low to neutralize the acidic contents of the duodenal lumen. Instead, the secretion of Brunner’s glands protects the duodenal mucosa – similar to the mucus which protects the gastric mucosa.
| Layer | Duodenum | Jejunum | Ileum |
| Serosa | 1st part serosa, 2nd – 4th adventitia | normal | normal |
| Muscularis externa | Longitudinal and circular layers, with Auerbach’s (myenteric) plexus in between | same as duodenum | same as duodenum |
| Submucosa | Brunner’s glands and Meissner’s (submucosal) plexus | no BG | no BG |
| mucosa: muscularis mucosae | normal | normal | normal |
| Mucosa: lamina propria | no Peyer’s patches | no Peyer’s patches | Peyer’s patches |
| Mucosa: intestinal epithelium | simple columnar. Contains goblet cells, Paneth cells | Similar to duodenum Villi very long | Similar to duodenum Villi very short |
Duodenum
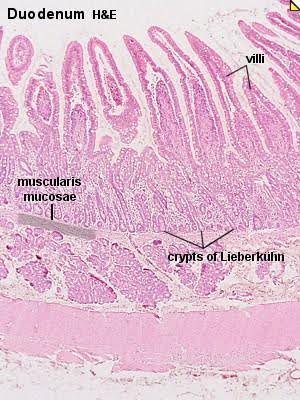
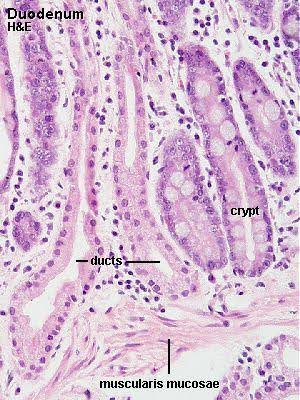
Duodenum – H&E
Take a close look at the epithelium lining the villi and crypts of the duodenum, and note the absence of plicae circulares.
Look at tall columnar epithelium composed of enterocytes, goblet cells and endocrine cells throughout the remainder of the GIT.
Identify the lamina propria and muscularis mucosae and the “packages” of glandular tissue (Brunner’s glands) in the connective tissue between the muscularis mucosae and muscularis externa, i.e. in the submucosa. Occasionally you will see ducts of Brunner’s gland which penetrate the muscularis mucosae and ascend through the lamina propria.
Note that goblet cells are absent from these ducts.
Jejunum – H&E
Look at the images and identify plicae circulares, muscularis externa and villi.
Next identify surface epithelium (simple columnar with goblet cells), crypts, and muscularis mucosae, submucosa and muscularis externa. Crypts will probably be smaller than you expect them from schematic drawings. They are fairly short and narrow.
Accumulations of lymphocytes are common in the mucosa of the GIT, and they occur frequently in the small intestine. They can form very large aggregates in particular in the ileum, where they may be covered by a specialized epithelium which facilitates their immune function (defense of the body against possible pathogens) in the lumen of the intestine. These specialized parts of the small intestine are called Peyer’s patches.
Movement: Peristalsis Segmentation MMC
The major mixing movement is segmentation, in which small, ringlike, contractions occur periodically, cutting the chyme into segments moving it back and forth. Peristaltic waves propel the chyme through the small intestine. These are weak waves so that the chyme moves slowly through the small intestine.
Secretions (Fluid/Enzymes/Hormones/Mucus):
- Dipeptidase, Aminopeptidase
- Crypts of Lieberkühn – water
- [Brunner’s glands]
- Alkaline mucus (protection)
- Epithelial cells- Crypts of Lieberkühn
- Mucus (lubricates and protect)
Disaccharidases:
- Lactase: lactose glucose + galactose
- Sucrase: sucrose glucose + fructose
- Maltase: maltose glucose+glucose
- Intestine lipase: fats glycerol + fatty acids
- Gastric inhibitory peptide: ↓ gastrin secretion and ↓ speed of gastric emptying (aka GIP)
- Enterokinase (trypsinogen trypsin, chymotrypsinogen chymotrypsin, and procarboxypolypeptidase carboxypolypeptidase)
- Bulbogastrone: ↓ parietal cell acid secretion
- S-cells: respond to ↓ pH, undigested fats
- Secretin: ↓gastrin secretion and motility, ↑bile salt secretion, ↑ pancreatic bicarbonate secretion, and ↓GI motility; protective function.
- I-cells: respond to undigested PRO’s and fats
Cholecystokinin
Cholecystokinin – abbreviated as CCK or CCK-PZ;
The word cholecystokinin comes from Greek chole, “bile”; cysto, “sac”; kinin, “move” 🡪 move the bile-sac.
Functions:
↓gastric motility, ↑ pancreatic enzyme to stimulate acinar cells, and bicarbonate secretion, and ↑gallbladder contraction, which stimulate bile; protective function.
Synthesized by I-cells in the mucosal epithelium of the small intestine and secreted in the duodenum, the first segment of the small intestine, and causes the release of pancreatic digestive enzymes and bile from the gallbladder. It also acts as a hunger suppressant.
The secretions of the intestinal mucosa are stimulated by the direct contact with chyme, which provides both chemical and mechanical stimuli, and by reflexes triggered by distention of the intestinal wall. It is inhibited by the lack of chyme in the small intestine.
Digestion
α-amylase from the pancreas almost totally converts all starches into maltose and other small glucose polymers.
All sugars such as lactose, sucrose, and maltose are broken down by their respective enzymes.
Peptidases in the cell membranes (aminopeptidase and dipeptidases) split the remainder of the larger polypeptides into tripeptides, dipeptides, and amino acids.
Phospholipids, cholesterol, and cholesterol esters are emulsified by bile (bile salts and lecithin)-lipase attacks the fat globules on their surfaces (pancreatic lipase and enteric lipase in enterocytes).
Absorption:
- Water by diffusion/ osmosis
- Sodium by Active Transport
- Chloride ions dragged by electrical gradient of:
- All monosaccharides except for fructose absorbed by secondary active transport w/Na+ mechanism dependent on sodium, fructose by facilitated diffusion.
- Amino Acids/peptides by the same route as monosaccharides (secondary active transport via Na+–5 transport proteins found.)
- Monoglycerides and free fatty acids diffuse immediately into the enterocytes.
Reflexes:
- Enterogastric reflex—the small intestine tells the stomach to slow down (negative feedback).
- Colonoilcal reflex
Innervation:
- Myenteric plexus (Auerbach’s plexus)
- Submucosal plexus (Meissner’s plexus)
- Parasympathetic
- Sympathetic
Disorders
- Abnormal digestion due to pancreatitis or blockage of pancreatic duct.
- Sprue—tropical—inflammation of the intestinal mucosa due to infectious bacterial agent/protozoan. (Treatment is difficult due to cyst form, eukaryote)
- Idiopathic/Celiac disease/gluten enteropathy—toxic effect of gluten present in certain types of grains and has a destructive effect on the enterocytes 🡪 steatorrhea and absorption impaired.
- Crohn’s Disease (esp. in ileum)
- Cystic fibrosis
- Hornip’s Disease
- Obstruction: interception, volvulus
- Disaccharide (lactose) intolerance
- Meconium Ileus: assoc. w/ pancreatic deficiency (precursor to CF)
Summary of each major type of digestive product and absorption site.
- Monosaccharides are absorbed by the villi by diffusion, facilitated diffusion, or active transport. The blood then carries them away.
- Amino acids are absorbed by the villi by means of active transport. The blood then carries them away.
- Fatty acids and glycerol are absorbed by diffusion into the lacteals of the villi. They are then carried away by lymph.
- Diffusion and active transport into the villi absorb electrolytes.
- Water is absorbed by osmosis into the villi.
Large Intestine
The cecum is a dilated, pouch like structure that hangs slightly below the ileocecal opening. This represents the beginning of the large intestine. The colon is divided into four parts. The ascending colon begins at the cecum and travels upward against the posterior abdominal wall to a point just below the liver. It turns sharply to the left and becomes the transverse colon. This is the longest and most movable part of the large intestine. As the transverse colon approaches the spleen, it turns abruptly downward and becomes the descending colon. At the brim of the pelvis, the descending colon makes an S-shaped curve, called the sigmoid colon, and then becomes the rectum. The rectum is firmly attached to the sacrum and it ends about five centimeters below the tip of the coccyx. It now is known as the anal canal. The anal canal is the last two and one-half to four centimeters of the large intestine. It ends at the anus, which opens to the outside of the body.
Functions of the large intestine
- It has little or no digestive function.
- It secretes mucous.
- Absorption is generally limited to water and electrolytes.
- Formation and storage of feces.
- Movement: Peristalsis-mass movement, Huastral (mixing)
- Secretions (Fluid/Enzymes/Hormones/Mucus)
- [Crypts of Lieberkühn]
- Mucus (lubrication, protection, solidification)
- Bicarbonate (neutralize bacterial products)
Digestion: None
Absorption: Water
Ions—Na+, K+, products of Vitamin K, intestinal Biotin, flora, (Almost no nutrients)
Reflexes
- Colonolileal reflex — the large intestine tells the small intestine to slow down (negative feedback).
- Gastrocolic reflex — signal from the stomach cause evacuation of the colon.
- Defecation reflex
- A person holds a deep breath and contracts the abdominal wall muscles. This increases the internal abdominal pressure and forces the feces into the rectum. As the rectal wall distends, this triggers the defecation reflex. Peristaltic waves in the descending colon are stimulated, and the internal anal sphincter relaxes. The external sphincter relaxes and the feces are forced to the outside.
Innervation:
- Parasympathetic
- Sacral
- Some Sympathetic
- (relax sphincter)
- Enteric nervous system
- Voluntary muscle contraction
Disorders:
- Constipation–anything that can obstruct the intestinal movements, irregular bowl habits, or spasm of the sigmoid colon.
- Megacolon/Hirschsprung’s disease — build-up of large quantity of fecal matter, lack of ganglion cells of the myenteric plexus in a segment of the sigmoid colon.
- Diarrhea- enteritis
- Crohn’s Disease
- Ulcerative Colitis
- Bacillary Dysentery
- Salivary glands—located in the oral cavity
- Saliva is secreted in large amounts (1-1.5 liters/day) by three pairs of exocrine salivary glands (parotid, submandibular, and sublingual) in the oral cavity, and is mixed with the chewed food by the tongue.
- The serous cells found in the salivary glands produce a watery fluid that contains amylase. Amylase is a digestive enzyme that splits starch and glycogen molecules into disaccharides. This is the first step of carbohydrate digestion.
- The parotid glands secrete a clear, watery fluid that is rich in amylase.
- The submandibular glands secrete a serous fluid with some mucous, making it more viscous than the parotid gland secretion.
- The sublingual glands secrete a thick and stringy mucous fluid
Liver
The liver is enclosed in a fibrous capsule and divided into lobes by connective tissue. Each lobe is further subdivided into hepatic lobules. These are the functional units of the liver. Each lobule consists of hepatic cells (hepatocytes) that radiate outward from a central vein.
Movement: None
Secretions (Fluid/Enzymes/Hormones/Mucus): Bile (emulsifies fats)
Digestion: None
Absorption: None
Reflexes: None
Innervation: Several
Disorders:
- Cirrhosis
- Hepatitis
- Storage diseases (all involve jaundice)
- Hemolytic/obstructive
- Cancer
Liver Functions:
- Metabolism
- Carbohydrate Metabolism
- Conversion of glucose to glycogen
- Breakdown of glycogen to glucose
- Protein Metabolism
- Deamination of amino acids & nucleic acids
- Lipid Metabolism
- Cholesterol metabolism
- Fat formation (glucose & amino acids)
- Fat breakdown
- Storage
- Glucose, stored as glycogen
- Bile storage in gallbladder
- Storage of Vitamins A, D, E, K, B1, B2, B12
- Fats & Fatty acids
- Water volume (blood volume)
Minerals: Iron & copper
Secretion & Synthesis
Secretion of bile salts into bile Bile is composed of bile salts, bile pigments (bilirubin and biliverdin), cholesterol, and electrolytes path of bile from a bile canal to the small intestine. The bile flows from the bile canal into hepatic ducts. The ducts then merge to form the common hepatic duct. It then can flow into the gallbladder for storage. The common hepatic and cystic duct form the common bile duct. This then empties into the duodenum. Bile salts emulsify fats and aid in the absorption of fatty acids, cholesterol, and certain vitamins.
Blood clotting factors
- Blood proteins
- Elaborates heparin
- Erythrocyte before birth
- Excretory Function
- Breakdown of hemoglobin
- Drug detoxification
- Breakdown of sterols
- Formation of urea from amino acids
- Blood buffering
- Detoxification
- Gallbladder
- Movement
- Contraction/constriction 🡪 stimulated by cholecystokinin, inhibited by Vagus nerve
Secretions (Fluid/Enzymes/Hormones/Mucus): Concentrated bile
Digestion: None
Absorption: None
Reflexes:
Innervation:
Disorders: Gallbladder stones
Gallstones form as a result of cholesterol precipitating out of solution and crystallizing. This can result if the bile becomes too concentrated, the hepatic cells secrete too much cholesterol, or the gallbladder is inflamed.
Pancreas
The pancreas is an elongated, somewhat flattened organ that is posterior to the stomach and behind the parietal peritoneum. It is attached to the duodenum by the pancreatic duct, which runs the length of the pancreas.
Movement: None
Secretions (Fluid/Enzymes/Hormones/Mucus):
- Bicarbonate and water
- Insulin and glucagon
- Enzymes & functions in pancreatic juice:
- Pancreatic amylase —digest carbohydrates
- Pancreatic lipase — digest triglycerides
- Trypsin — digest protein
- Chymotrypsin —digest protein
- Carboxypeptidase — digest protein
- Nucleases—break nucleic acids into nucleotides
Absorption: none
Reflexes:
- Secretin stimulates the release of pancreatic juice that has a high bicarbonate ion concentration.
- Cholecystokinin stimulates the release of pancreatic juice that has a high concentration of digestive enzymes.
- Acidic chyme in the duodenum triggers the release of pancreatic juice. As the chyme moves through the intestine the pancreatic juice is inhibited.
Innervation:
Disorders:
- Pancreatitis
- Pancreatic cancer
- Mechanism of vomiting
Sensory impulses travel from the site of stimulation to the vomiting center in the medulla oblongata, and a number of motor responses follow. These include taking a deep breath, raising the soft palate and thus closing the nasal cavity, closing the opening to the trachea (glottis), relaxing the circular muscle fibers at the base of the esophagus, contracting the diaphragm so that it moves downward over the stomach, and contracting the abdominal wall muscles so that pressure inside the abdominal cavity increases. As a result, the stomach is squeezed from all sides, forcing its contents upward and out through the esophagus, pharynx, and mouth.
Effects of Aging on the Digestive Tract
Altered rates of absorption in the small intestine
Because the small intestine is the site of absorption of nutrients, it is here that noticeable signs of aging on digestion arise. Subtle shifts in the microbial species that inhabit the small intestine alter the rates of absorption of particular nutrients. With age, the small intestine becomes less efficient at absorbing vitamins A, D, and K and the mineral zinc. This raises the risk of deficiency symptoms—effects on skin and vision due to a lack of vitamin A; weakened bones from inadequate vitamin D; impaired blood clotting seen in vitamin K deficiency; and slowed healing, decreased immunity, and altered taste evidenced in zinc deficiency.
Digestive function
- Older people sometimes do not chew food thoroughly because thinning enamel makes teeth more sensitive to hot and cold foods, gums recede, and teeth may loosen.
- Slowing peristalsis in the digestive tract may cause heartburn and constipation.
- Aging affects nutrient absorption in the small intestine.
- Accessory organs to digestion also age, but not necessarily in ways that affect health.
Laboratory Activity: Macroscopic Anatomy
Use the anatomical models available in the lab to identify the following structures:
| STRUCTURES | ✔️ | X |
| Mouth | ||
| Tongue | ||
| Papilla | ||
| Hard palate | ||
| Soft palate | ||
| Lingual frenulum | ||
| Upper lip | ||
| Lower lip | ||
| Maxillary teeth | ||
| Mandibular teeth | ||
| Salivary glands | ||
| Parotid gland | ||
| Submandibular gland | ||
| Sublingual gland | ||
| Pharynx | ||
| Esophagus | ||
| Stomach | ||
| Cardia | ||
| Greater curvature | ||
| Lesser Curvature | ||
| Fundus | ||
| Body | ||
| Pylorus | ||
| Stomach rugae | ||
| Gastric pits – microscope slides | ||
| Simple columnar epithelium | ||
| Small Intestine – villi | ||
| Duodenum | ||
| Jejunum | ||
| Ileum | ||
| Cecum | ||
| Vermiform appendix | ||
| Ascending colon | ||
| Transverse colon | ||
| Descending colon | ||
| Sigmoid colon | ||
| Rectum | ||
| Anus | ||
| Anal sphincter | ||
| Liver | ||
| Right lobe | ||
| Left Lobe | ||
| Caudate lobe | ||
| Quadrate lobe | ||
| Hepatic portal vein | ||
| Hepatic artery | ||
| Right hepatic duct | ||
| Left hepatic duct | ||
| Common hepatic duct | ||
| Cystic duct | ||
| Common bile duct | ||
| Gallbladder | ||
| Pancreas | ||
| Pancreatic duct | ||
| Tooth | ||
| Crown | ||
| Neck | ||
| Root | ||
| Gingiva | ||
| Enamel | ||
| Dentin | ||
| Cementum |
Microscopic Anatomy
Obtain microscope slides from your instructor. View them under scanning power to locate the sample, then increase magnification up to 40X. Draw and label each of them.
- Esophagus: identify the lumen, non- keratinized stratified squamous epithelium, lamina propria, muscularis mucosae, submucosa, submucosal mucous glands, muscularis externa (all smooth muscle), and adventitia layer.
Simple squamous epithelium Magnification ___________X
For online labs, go to University of Michigan, virtual microscope: Full Slide List or scan the QR code.

Search for slide #153 – Esophagus, H&E, 20X.
- Stomach: identify the gastric glands, simple columnar epithelium, smooth muscle layers.
For online labs, go to University of Michigan, virtual microscope: Full Slide List or scan the QR code.


Search for slide #156 – Stomach, H&E, 20X.
Pits, glands, mucous cells, parietal cells [acid], chief cells [pepsinogen], muscularis mucosae, submucosa, muscularis).
Small intestines: duodenum, identify the duodenal glands, plica, simple columnar epithelium with Goblet cells, smooth muscle layers
Slide 162 – Small intestine, duodenum [right side of section], H&E, 40X (villi very poorly preserved, glands [crypts of Lieberkühn], muscularis mucosae, submucosal glands).
Small intestines – jejunum, identify, plica, simple columnar epithelium with Goblet cells, smooth muscle layers

Small intestines – ileum, identify the Peyer Patches, plica, simple columnar epithelium with Goblet cells, smooth muscle layers

Large intestines, identify the epithelium, simple columnar epithelium with Goblet cells, intestinal crypts.

Media Attributions
- Digestive system diagram © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Primary teeth © Maria Carles is licensed under a CC BY-SA (Attribution ShareAlike) license
- Permanent teeth © Studio Dentaire is licensed under a All Rights Reserved license
- Histological structure of a tooth © Maria Carles is licensed under a CC BY-SA (Attribution ShareAlike) license
- Intestinal villi and crypts of Lieberküh © By Nephron - Own work, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=7823376 is licensed under a CC BY-SA (Attribution ShareAlike) license
- Blank circle
- QR code V Microscope © Maria Carles is licensed under a CC BY-SA (Attribution ShareAlike) license
- Esophagus, H&E, 20X © Maria Carles adapted by Michigan Medical School is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Stomach, H&E, 20X © Maria Carles is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license