The Bone Tissue
Introduction to Skeletal System Laboratory Activity
Introduction
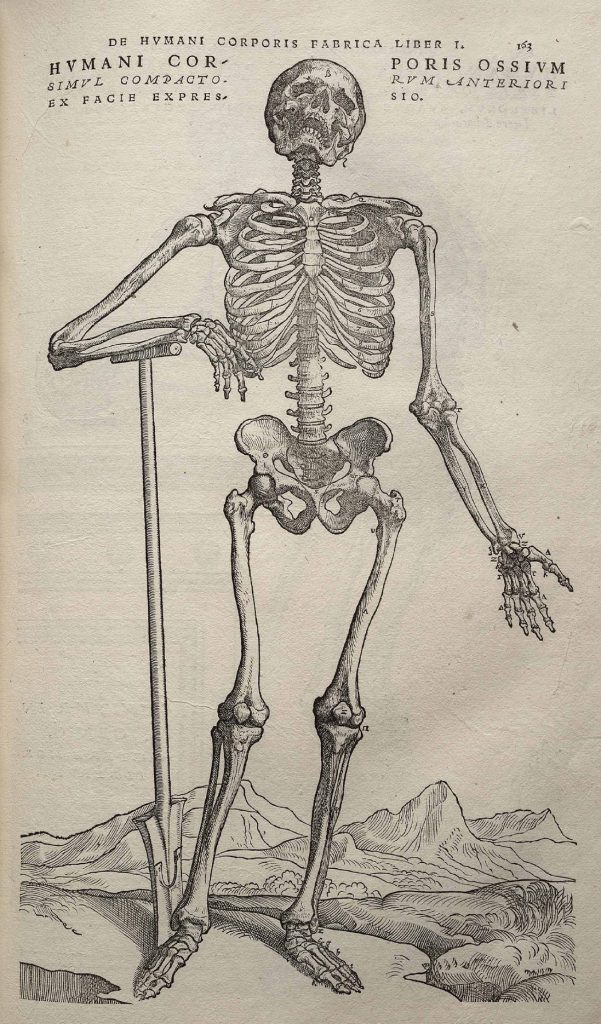
The skeletal system consists of bones and cartilages in the body.
Bones are complex organs, they are made up of bone cells, protein fibers, minerals, and other types of tissues. The main function of the skeletal system is to provide support and protection to the soft tissues that make up the rest of the body. The skeletal system also provides attachment for muscles to allow movements at the joints, it is a place where store fat and precious minerals such as calcium and phosphorous. Another function of bones is to house the bone marrow that is involved in the production of the formed element of blood.
In the human body at birth, there are over 300 bones, many of these bones fuse together during development, leaving a total of 206 separate bones in the adult, not counting numerous small sesamoid bones. The largest bone in the body is the femur or thigh-bone, and the smallest is the stapes in the middle ear.
This laboratory exercise will introduce you to the components of bone, its functional units and the skeletal system as a whole. You will also learn to identify the shape of bones that form the human skeleton and selected processes of the bones.
Objectives
- List major functions of the human skeletal system
- Describe and list types of bones
- Identify and label the structural and functional units of osseous tissue at the microscopic level
- Classify bones according to shape, and give examples of each
- Identify parts of long bones and flat bones
- List and describe the function of selected bone markings
Part 1 – Osseous Tissue
Bone tissue (osseous tissue) is a hard and mineralized connective tissue, it is made up of different types of bone cells: osteoblasts and osteocytes are involved in the formation and mineralization of bone; osteoclasts are involved in the resorption of bone tissue. Modified (flattened) osteoblasts become the lining cells that form a protective layer on the bone surface.
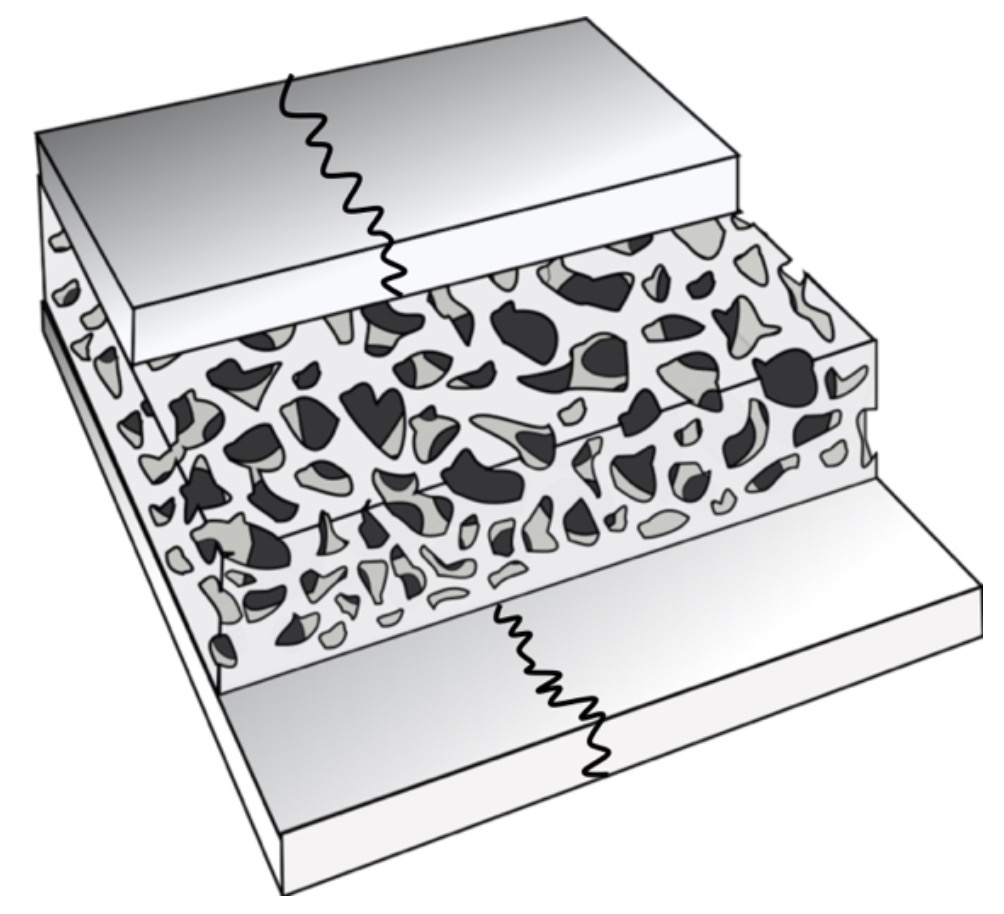
The mineralized matrix of bone tissue has an organic component of mainly collagen called ossein and an inorganic component of bone mineral made up of various salts . There are two types of mineralized bone; Compact bone (cortical) and Spongy (trabecular or cancellous) bone.
Bone is not uniformly solid, it consists of a flexible matrix and bound minerals, which are intricately woven and endlessly remodeled by a group of specialized bone cells. Their unique composition and design allow bones to be relatively hard and strong, while remaining lightweight.
Bone matrix is 90 to 95% composed of elastic collagen fibers, also known as ossein and the remainder is ground substance. The elasticity of collagen improves fracture resistance. The matrix is hardened by the binding of inorganic mineral salt calcium phosphate in a chemical arrangement known as calcium hydroxyapatite. It is the bone mineralization that give bones rigidity.
Bone is actively constructed and remodeled throughout life by special bone cells known as osteoblasts and osteoclasts. Within any single bone, the tissue is woven into two main patterns, known as cortical and cancellous bone, and each with different appearance and characteristics.
Compact or Cortical bone
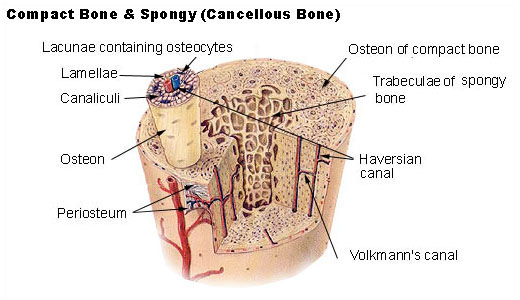
The hard, outer layer of bones is composed of cortical bone also called compact bone being much denser than cancellous bone. The cortical bone gives bone its smooth, white, and solid appearance, and accounts for 80% of the total bone mass of an adult human skeleton. It facilitates bone’s main functions: to support the whole body, protect organs, provide levers for movement, and store and release minerals, mainly calcium and phosphorus. It consists of multiple microscopic functional units, called an osteon.
The osteons (Harvesian Systems) are arranged as multiple layers of osteoblasts and osteocytes around a central canal or Haversian canal. The osteons connect with each other at right angles via the perpendicular or Volkmann’s canals. Osteons are metabolically active, and as bone is reabsorbed and created the nature and location of the cells within the bone will change. Cortical bone is covered by a periosteum on its outer surface, and an endosteum on its inner surface. The endosteum is the boundary between the cortical bone and the cancellous bone. The periosteum is formed of two layers: the outer fibrous layer made of dense irregular fibrous connective tissue where the blood vessels and nerves are located and the inner cellular layer of periosteum that contains osteogenic cells that become osteoblasts (build the matrix) and osteoclasts (reabsorb the matrix). The fibers of the periosteum extend to form Sharpey’s fibers that anchor the periosteum to the bone.
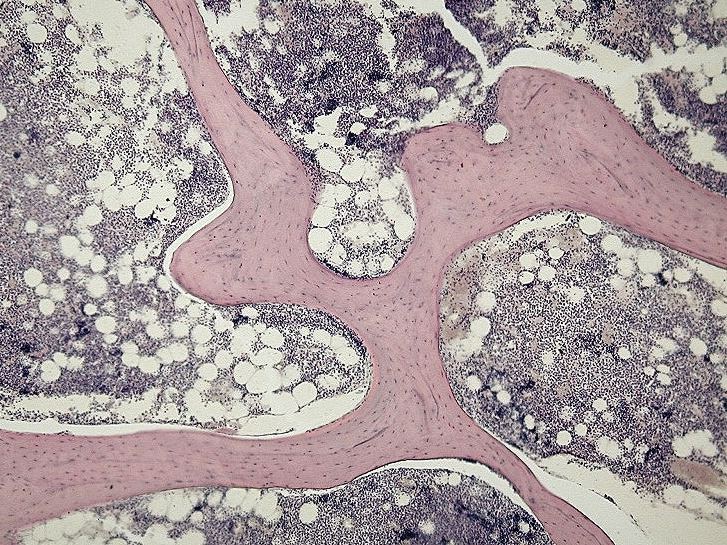
Cancellous bone, also called trabecular or spongy bone, is the internal tissue of the skeletal bone and is an open cell porous network. Cancellous bone has a higher surface-area-to-volume ratio than cortical bone because it is less dense. This makes it weaker and more flexible. The greater surface area also makes it suitable for metabolic activities such as the exchange of calcium ions. Cancellous bone is typically found at the ends of long bones, near joints and in the interior of vertebrae. Cancellous bone is highly vascular and often contains red bone marrow where hematopoiesis, the production of blood cells, occurs. The primary anatomical and functional unit of cancellous bone is the trabecula. The trabeculae are aligned towards the mechanical load distribution that a bone experiences within long bones such as the femur. As far as short bones are concerned, trabecular alignment has been studied in the vertebral pedicle. Thin formations of osteoblasts covered in endosteum create an irregular network of spaces, known as trabeculae. Within these spaces are bone marrow and hematopoietic stem cells that give rise to platelets, red blood cells and white blood cells. Trabecular marrow is composed of a network of rod- and plate-like elements that make the overall organ lighter and allow room for blood vessels and marrow. Trabecular bone accounts for the remaining 20% of total bone mass but has nearly ten times the surface area of compact bone.
The words cancellous and trabecular refer to the tiny lattice-shaped units (trabeculae) that form the tissue.
Bone marrow
Bone marrow, also known as myeloid tissue in red bone marrow, can be found in almost any bone that holds cancellous tissue. In newborns, all such bones are filled exclusively with red marrow, but as the child ages the hematopoietic fraction decreases in quantity and the fatty/ yellow fraction called marrow adipose tissue (MAT) increases in quantity. In adults, red marrow is mostly found in the bone marrow of the femur, the ribs, the vertebrae and pelvic bones.
Bone cells
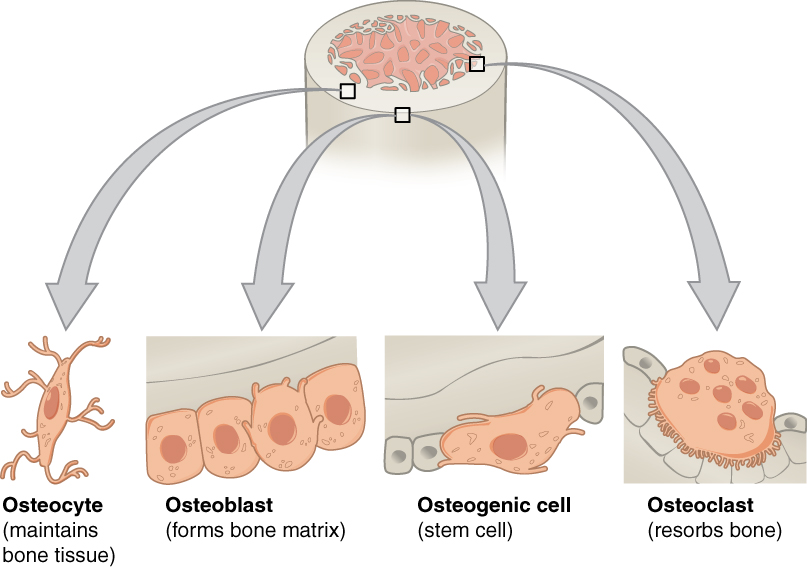
Bone is a metabolically active tissue composed of several types of cells. These cells include osteoblasts, which are involved in the creation and mineralization of bone tissue, osteocytes, and osteoclasts, which are involved in the reabsorption of bone tissue.
Osteoblast
Osteoblasts are mononucleate bone-forming cells. They are located on the surface of osteon seams and make a protein mixture known as osteoid, which mineralizes to become bone.
The osteoid seam is a narrow region of newly formed organic matrix, not yet mineralized, located on the surface of a bone. Osteoid is primarily composed of Type I collagen. Osteoblasts also manufacture hormones, such as prostaglandins, to act on the bone itself. The osteoblast creates and repairs new bone by actually building around itself. First, the osteoblast puts up collagen fibers. These collagen fibers are used as a framework for the osteoblasts’ work. The osteoblast then deposits calcium phosphate which is hardened by hydroxide and bicarbonate ions. The brand-new bone created by the osteoblast is called osteoid. Once the osteoblast is finished working it is actually trapped inside the bone once it hardens. When the osteoblast becomes trapped, it becomes known as an osteocyte. Other osteoblasts remain on the top of the new bone and are used to protect the underlying bone, these become known as lining cells.
Osteocyte
Osteocytes are mostly inactive osteoblasts. Osteocytes originate from osteoblasts that have migrated into and become trapped and surrounded by bone matrix that they themselves produced. The spaces they occupy are known as lacunae. Osteocytes have many processes that reach out to meet osteoblasts and other osteocytes probably for the purposes of communication. Osteocytes remain in contact with other cells in the bone through gap junctions—coupled cell processes—which pass through small channels in the bone matrix called the canaliculi.
Osteoclast
Osteoclasts are very large multinucleate cells that are responsible for the breakdown of bones by the process of bone resorption. New bone is then formed by the osteoblasts. Bone is constantly remodeled by the resorption of osteoclasts and created by osteoblasts. Because the osteoclasts are derived from a monocyte stem-cell lineage, they are equipped with phagocytic-like mechanisms similar to circulating macrophages. Osteoclasts mature and/or migrate to discrete bone surfaces. Upon arrival, active enzymes, such as tartrate resistant acid phosphatase, are secreted against the mineral substrate. The reabsorption of bone by osteoclasts also plays a role in calcium homeostasis.
Extracellular matrix
Bones consist of living cells embedded in a mineralized organic matrix. This matrix consists of organic components, mainly type I collagen – “organic” referring to materials produced as a result of the human body – and inorganic components, primarily hydroxyapatite and other salts of calcium and phosphate. Above 30% of the acellular part of bone consists of the organic components, and 70% of salts. The collagen fibers give bone its tensile strength, and the interspersed crystals of hydroxyapatite give bone its compressive strength. These effects are synergistic.
The inorganic composition of bone (bone mineral) is primarily formed from salts of calcium and phosphate, the major salt being hydroxyapatite (Ca10(PO4)6(OH)2). The exact composition of the matrix may be subject to change over time due to nutrition and biomineralization, with the ratio of calcium to phosphate varying between 1.3 and 2.0 (per weight), and trace minerals such as magnesium, sodium, potassium and carbonate also being found.
Type I collagen composes 90–95% of the organic matrix, with remainder of the matrix being a homogenous liquid called ground substance consisting of proteoglycans such as hyaluronic acid and chondroitin sulfate, as well as non-collagenous proteins such as osteocalcin, osteopontin or bone sialoprotein. Collagen consists of strands of repeating units, which give bone tensile strength, and are arranged in an overlapping fashion that prevents shear stress.
Part 2 – Classification of Bones Based on Shape
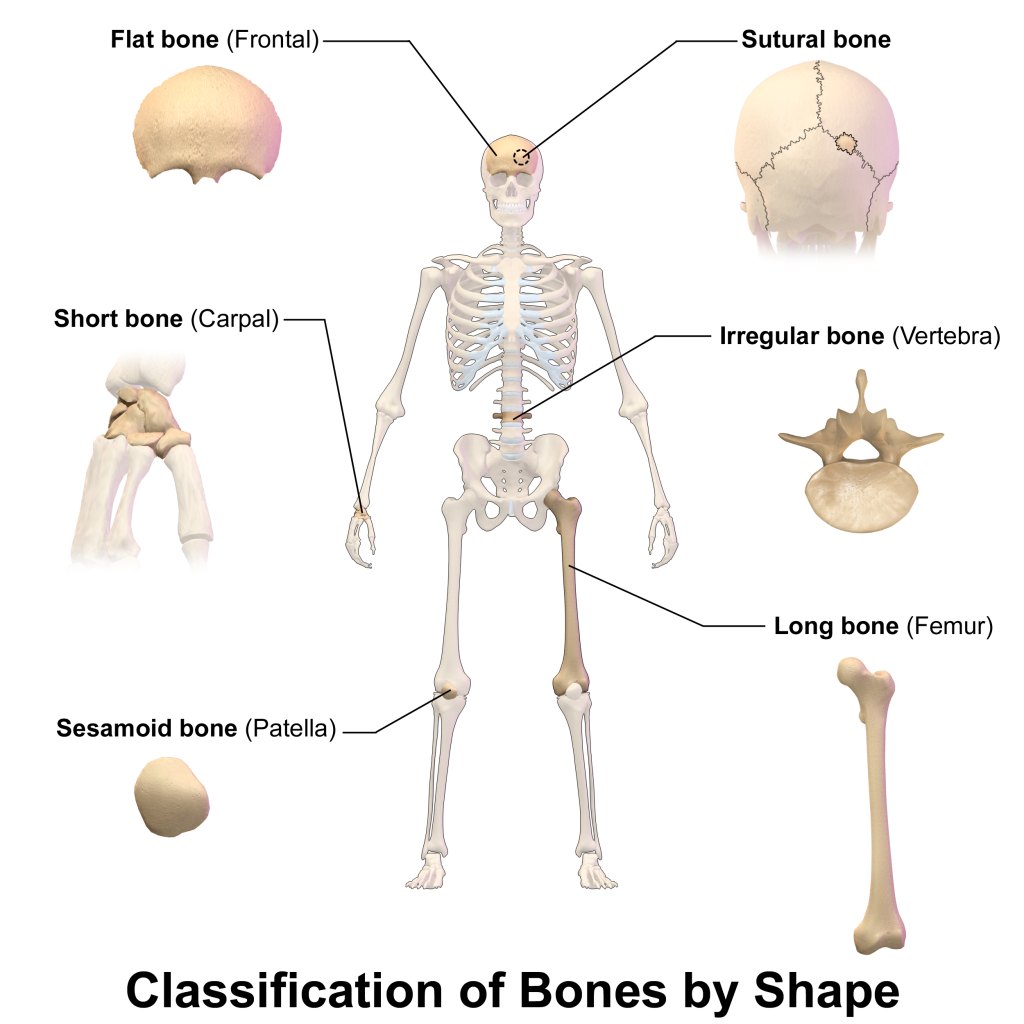
There are six types of bones in the human body: long, short, flat, irregular, sesamoid and sutural.
Watch the following animation “Bone Shape – Drawn and Defined”
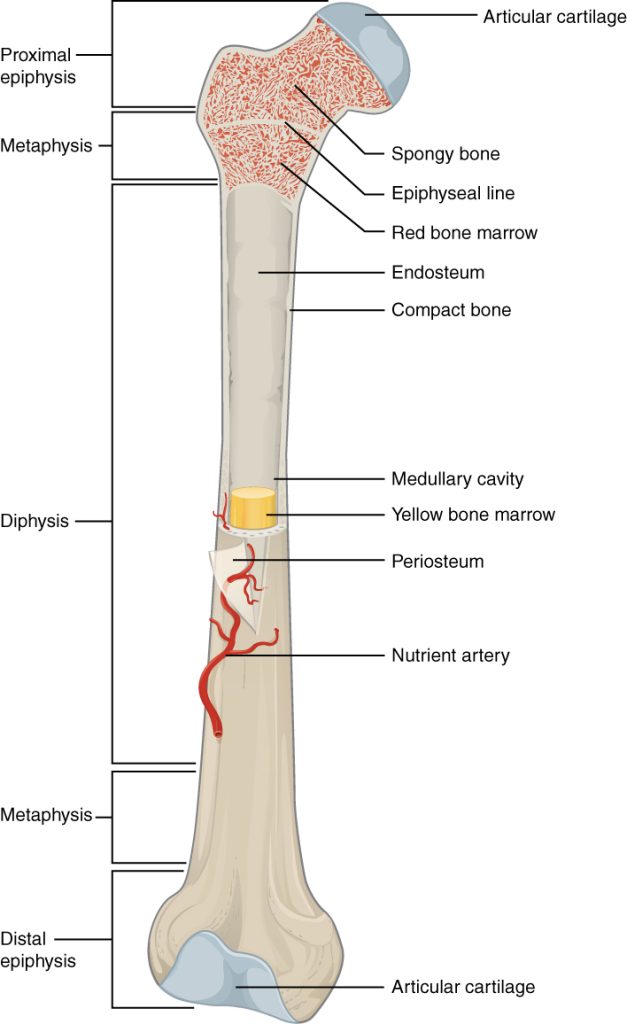
Long bones are characterized by a shaft, the diaphysis, that is much longer than its width; and by an epiphysis, a rounded head at each end of the shaft. They are made up mostly of compact bone, with lesser amounts of marrow, located within the medullary cavity, and areas of spongy, cancellous bone at the ends of the bones. Most bones of the limbs, including those of the fingers and toes, are long bones. The exceptions are the eight carpal bones of the wrist, the seven articulating tarsal bones of the ankle and the sesamoid bone of the kneecap. Long bones such as the clavicle, that have a differently shaped shaft or ends are also called modified long bones.
Short bones are roughly cube-shaped and have only a thin layer of compact bone surrounding a spongy interior. The bones of the wrist and ankle are short bones.
Flat bones are thin and generally curved, with two parallel layers of compact bones sandwiching a layer of spongy bone. Most of the bones of the skull are flat bones, as is the sternum.
Sesamoid bones are bones embedded in tendons. Since they act to hold the tendon further away from the joint, the angle of the tendon is increased and thus the leverage of the muscle is increased. Examples of sesamoid bones are the patella and the pisiform.
Irregular bones do not fit into the above categories. They consist of thin layers of compact bone surrounding a spongy interior. As implied by the name, their shapes are irregular and complicated. Often this irregular shape is due to their many centers of ossification or because they contain bony sinuses. The bones of the spine, pelvis, and some bones of the skull are irregular bones. Examples include the ethmoid and sphenoid bones.
Sutural bones are small bones located between flat bones of the skull at the suture.
Also called Wormian bones.
Watch the animation “Anatomy of long bones”
Table 1 – Summary of Bone Shapes
| Shape | Description | Example |
| Long bones | Longer that they are wide | Humerus, radius, ulna, femur, tibia fibula |
| Short bones | Length and wide are about the same | Bones of the wrist and ankle |
| Flat bones | They are flat | Bones of the skull, sternum, ribs, and hip |
| Irregular bones | Shape does not fit any of the other descriptions | Ethmoid, sphenoid bone, vertebra, sacrum |
| Sesamoid bones | Oval shaped bones located within tendons | Patella |
| Sutural bones | Small bones located between flat bones of the skull at the suture | Wormian bones of skull |
Part 3 – Bone Markings
Bone markings are very important, they allow the identification of bones and bony pieces. Bone markings enable joints to form, to slide past each other, to lock bones in place, and to provide a place of attachment and structural support to muscle and connective tissue. They also provide stabilization, protection and a pathway to nerves, vessels, and other structures.
Bone markings consist of depressions, openings and projections.
Depressions provide pathways for blood vessels and nerves to travel to their target; they also allow two bones to form a joint. Opening houses and protecting structures. Projections provide points of attachment for muscles via tendons and bone to bone via ligaments.
Common Bone Markings Include the Following:
- Angles – Sharp bony angulations which may serve as bony or soft tissue attachments. Examples include the superior, inferior, and acromial angles of the scapula and the superior, inferior, lateral angles of the occipital bone, and the angle of the mandible.
- Body – Usually refers to the largest most prominent segment of bone. Examples include the diaphysis or shaft of long bones like the femur and humerus and the body of the mandible.
- Canal – passageway through a bone.
- Condyle – Refers to a large rounded prominence which often provides structural support to the overlying hyaline cartilage. Examples include the knee joint, formed by the femoral lateral and medial condyles, and the tibial lateral and medial condyles and occipital condyle which allows the articulation of the occipital bone and the atlas (C1).
- Crest – A raised or prominent part of the edge of a bone. Crests are often the sites where connective tissue attaches muscle to bone. An example is the iliac crest found on the ilium.
- Epicondyle – A prominence that sits atop of a condyle. The epicondyle attaches muscle and connective tissue to bone, providing support to this musculoskeletal system. Examples include the femoral medial and lateral epicondyles, and humeral medial and lateral epicondyles.
- Facet – A smooth, flat surface where two bones meet to form a joint. Examples include the facet joints of the vertebrae for flexion and extension of the spine.
- Fissure – An open slit in or between bones. It usually houses nerves and blood vessels. Examples include superior and inferior orbital fissures.
- Foramen – A hole in a bone through which nerves and blood vessels pass. Examples include foramen magnum, supraorbital foramen, infraorbital foramen, and mental foramen.
- Fossa – A shallow depression in a bone surface. Examples include trochlear fossa, posterior, middle, and anterior cranial fossa.
- Fovea – Shallow pit that allows the attachment of a ligament.
- Groove – A long shallow depression on the bone surface that usually allows a blood vessel or nerve to travel along the length of the bone. Examples include a radial groove.
- Head – A rounded end of a bone, it is a prominent extension of bone that forms part of a joint. Example the head of the radius and the femur.
- Line – Ridge along a bone that allows a muscle to attach to the bone.
- Margin – The edge of any flat bone. For example, the edge of the temporal bone articulating with the occipital bone is called the occipital margin of the temporal bone.
- Meatus – A tube-like channel that extends within the bone, which may provide passage and protection to nerves, vessels, and sound. Examples include external acoustic meatus and internal auditory meatus.
- Neck – The segment between the head and the shaft of a bone. For example, the anatomical neck of the humerus.
- Notch – A depression in a bone which often provides stabilization to an adjacent articulating bone. Examples include the trochlear notch on the ulna, radial notch of the ulna, suprasternal notch, and the mandibular notch.
- Process – bony projection, allows for muscle attachment.
- Protuberance – A bump or outgrowth on a bone.
- Ramus – The curved part of a bone that gives structural support to the rest of the bone. Examples include the ramus of the mandible.
- Sinus – A cavity within a bone. Examples include paranasal sinuses.
- Spinous Process – A raised, sharp elevation of bone where muscles and connective tissue attach. Example spinous process of the vertebra.
- Sulcus – Same as groove
- Trochanter – A large prominence on the side of the bone. Some of the largest muscle groups and most dense connective tissues attach to the trochanter. The most notable examples are the greater and lesser trochanters of the femur.
- Tubercle – A small, rounded prominence where connective tissues attach. Examples include the greater and lesser tubercle of the humerus.
- Tuberosity – A moderate prominence where muscles and connective tissues attach. Its function is similar to that of a trochanter. Examples include the tibial tuberosity, deltoid tuberosity, and ischial tuberosity.
Laboratory Activity
Part 1 – Osseous Tissue
- Identify and label the structures of compact bone using the diagram of Anatomical Model of Bone.
- Structures: Periosteum, Sharpey’s fibers, Circumferential lamellae, Osteon, Central Canal, Osteocytes, Lacunas, Canaliculi, Perforating canals, Concentric lamellae, Interstitial lamellae, Endosteum, Bone marrow.
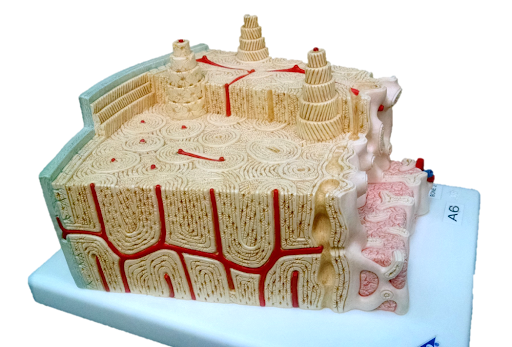
- Structures: Periosteum, Sharpey’s fibers, Circumferential lamellae, Osteon, Central Canal, Osteocytes, Lacunas, Canaliculi, Perforating canals, Concentric lamellae, Interstitial lamellae, Endosteum, Bone marrow.
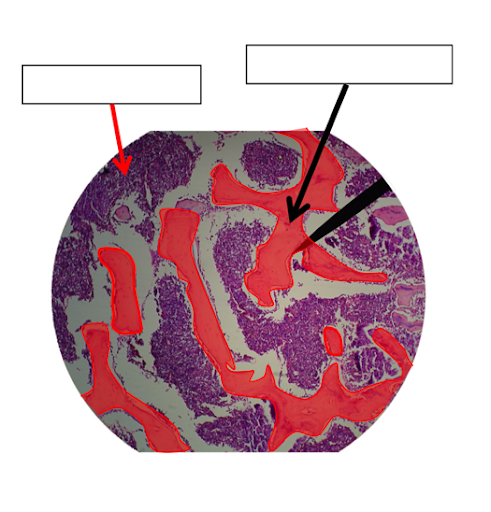
- View a slide of spongy bone. In a standard face to face lab, use the microscope and available slides – spongy or trabecular bone.
- 100% online mode – Instead of using the standard compound light microscope, you will use the University of Michigan (UM) “Virtual Microscope”.
- Go to University of Michigan Histology and Virtual Microscopy Learning Resources
- Click on “Digital Microscopy” and review the instructions on how to use the Virtual Microscope (Zoomify).
- Next, go to Virtual Slide List
- Search for “spongy bone”
- Or you can click on the image shown below (links already embedded), scan for the tissue you need to see, then Zoomify using the +/- controls (below the image) and draw the tissues in your notebook or space provided.
- You may also scan the image – look at the top left of the main view, you will see a smaller window with a blue square, drag the square to change the area where you like to see. You can also move to a different area in the main view by dragging the small white hand shown there.
Slide: 048_HISTO_40X

Focus on the area where spongy bone (blue arrow) is located and zoom in.
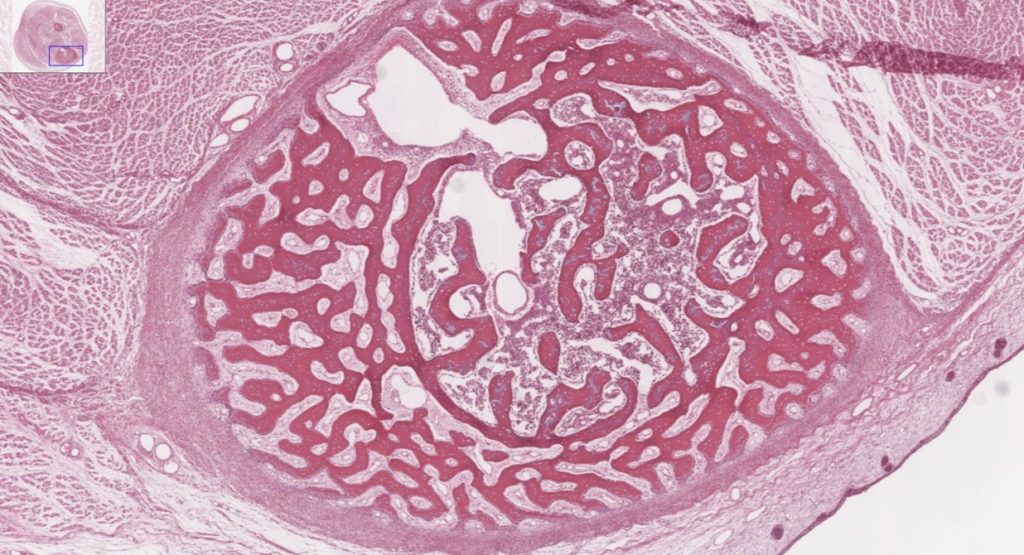
- Label spongy bone structures shown in this micrograph (arrows): trabecula, bone marrow.
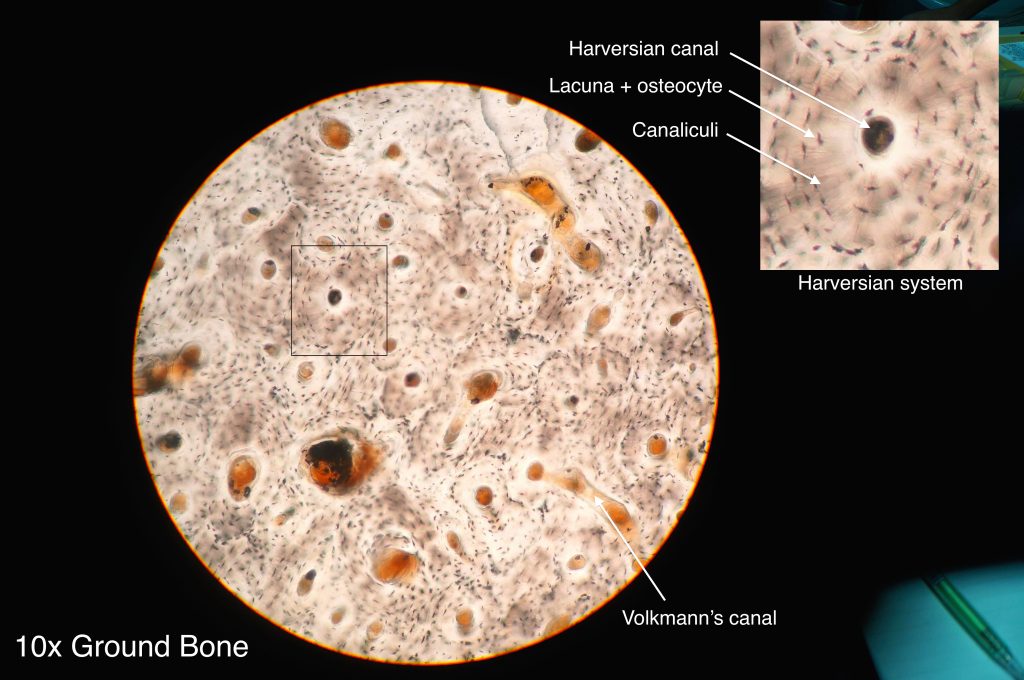
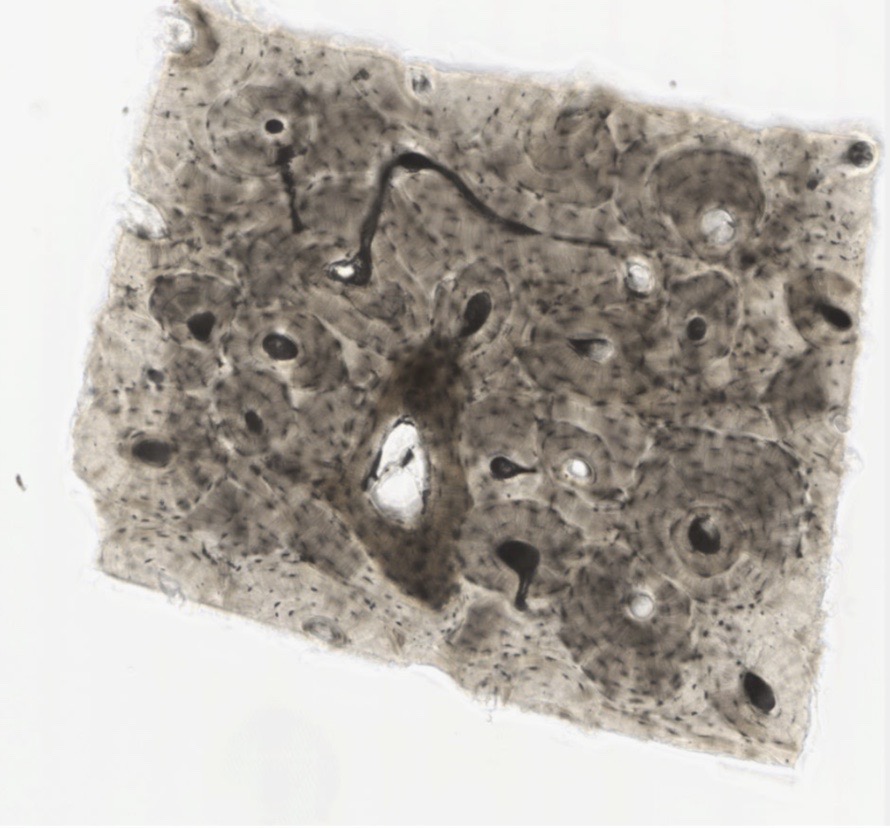
- Compact bone – View a slide of compact bone. In a standard face to face lab, use the microscope and available slides – ground compact bone.
- 100% online mode – Instead of using the standard compound light microscope, you will use the University of Michigan (UM) “Virtual Microscope”.
- Go to University of Michigan Histology and Virtual Microscopy Learning Resources or QR code below.

- Click on “Digital Microscopy” and review the instructions on how to use the Virtual Microscope (Zoomify).
- Next, go to Virtual Slide List
- Search for “compact bone”
- Or you can click on the image shown below (links already embedded), scan for the tissue you need to see, then Zoomify using the +/- controls (below the image) and draw the tissues in your notebook or space provided.
- You may also scan the image – look at the top left of the main view, you will see a smaller window with a blue square, drag the square to change the area where you like to see. You can also move to a different area in the main view by dragging the small white hand shown there. You will use two images:
- Ground compact bone Thin section #093A
- Ground compact bone #093B

- Slide: #093A
- Go to University of Michigan Histology and Virtual Microscopy Learning Resources or QR code below.
- Use the following link to use the UM virtual microscope. You download the image at low and high-power magnification.
Slide: #093B - Label the structures of compact bone shown in this micrograph (look for the numbers- some white others red)
- At low magnification label the following:
Osteon
Circumferential lamella
Interstitial Lamella,
Central CanalAt high magnification label the following: Canaliculi, Osteocytes, Lacuna,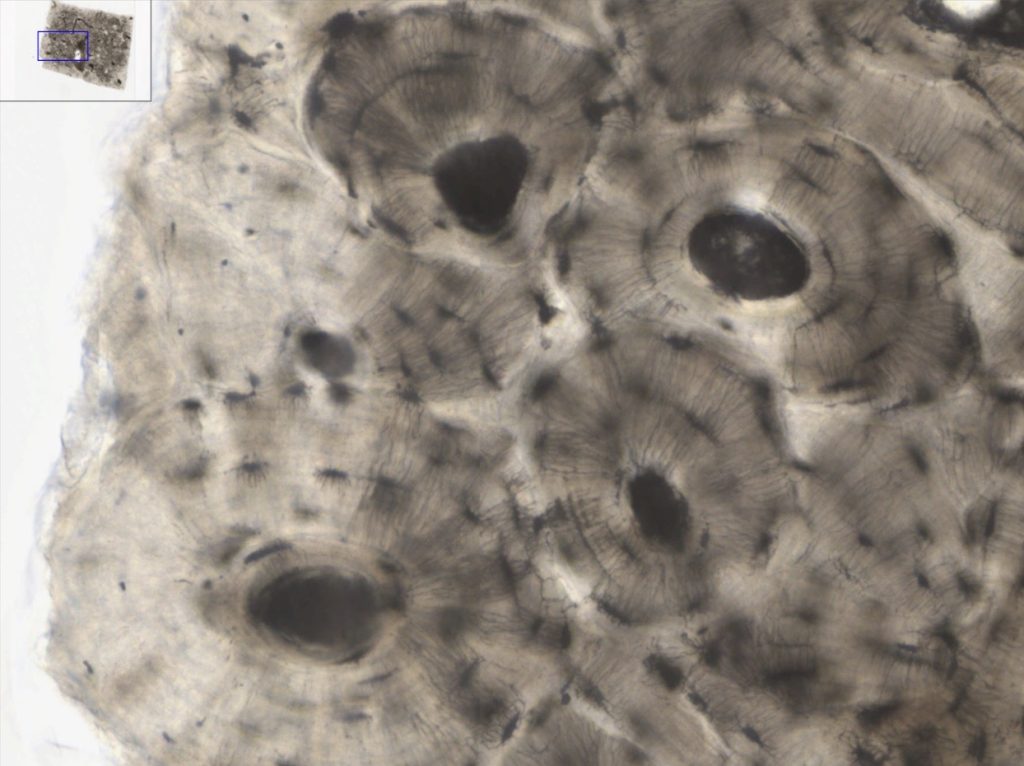
The image highlights the dense structure of compact bone, focusing on osteons and Haversian systems visible at high magnification. - Use the following link to use the UM virtual microscope. You download the image at low and high-power magnification.
Slide: #051 – longitudinal section of compact bone

- At low magnification label the following:
Central Canal
Volkman’s canal
Part 2 – Identify Bones Shapes
- Using your textbook, identify the shape of the bones shown here: long, short, flat, sesamoid or irregular.
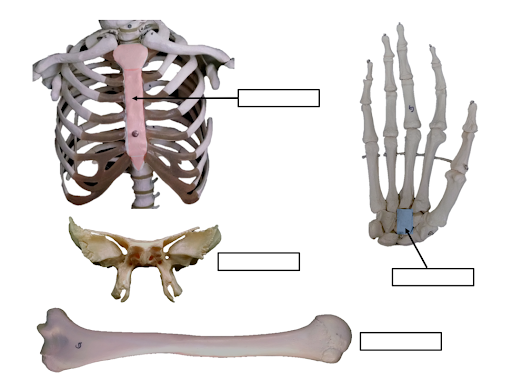
- Fill in the table shown below and give at least 3 examples of each.
Table 2 – Bone Shapes
| Shape | Description | Example |
| Long bones | ||
| Short bones | ||
| Flat bones | ||
| Irregular bones | ||
| Sesamoid bones | ||
| Sutural bones |
Part 3 – Anatomy of Long and Flat Bones
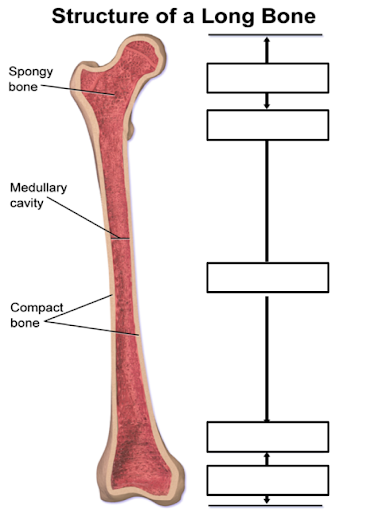
- Label the structures of a long bone shown below
- Label the structures of a flat bone show bellow: Trabeculae, spongy bone, compact bone, suture
Part 4 – Identifying Bone Markings
Identify bone markings
In a standard face to face lab, we will work in groups of two. In a 100% lab you will work individually.
Standard face to Face
- Obtain a disarticulated bone set.
- Organize the bones according to shape. Please note that you may have to look around the lab for missing bones from your box, or you may have more bones that you should, that is because the group that use the box before you were not very careful and organized, do not get discouraged, the bones are in the lab, you just need a few minutes to find them and make sure you have a complete set.
- Examine each bone and find one of the selected bone markings described in this lab exercise (pages 11-12), you may need to refer to your textbook for help.
- Write at least one bone marking found per selected bone, use the table provided to complete the activity.
100% online labs – look for images of all bones shown below, take a picture with your phone, download them and upload them here with their respective names and bone marking– see table below.
Table 3 – Bone markings
| Bones | Markings of bone |
| Frontal bone | |
| Occipital bone | |
| Temporal bone | |
| Vertebra | |
| Mandible | |
| Sternum | |
| Clavicle | |
| Scapula | |
| Ribs | |
| Humerus | |
| Radius | |
| Ulna | |
| Ilium | |
| Ischium | |
| Pubis | |
| Femur | |
| Tibia | |
| Fibula |
Part 5 – Review Key Terms
At the end of this activity you should be able to identify the following:
- Long bone anatomy:
- Periosteum
- Endosteum
- Diaphysis (shaft)
- Epiphyses, proximal and distal
- Metaphyseal line
- Perforating fibers
- Nutrient artery
- Spongy bone
- Compact bone
- Medullary cavity
- Articular cartilage
- Red marrow
- Yellow marrow
- Epiphyseal line
- Histology of Bone Tissue Models:
Compact bone
-
- Osteon
- Concentric lamellae
- Interstitial lamellae
- Circumferential lamellae
- Haversian canal
- Osteocyte
- Lacunae
- Canaliculi
- Perforating canal
- Periosteum
- Sharpey’s fibers
Spongy bone
-
- Trabeculae
- Endosteum
- Lamella
Hyaline cartilage
-
- Perichondrium
- Matrix
- Chondrocyte
- Lacunae
- Bone Shapes
-
- Long
- Short
- Flat
- Irregular
- Sesamoid
- Sutural
- Bone markings
-
- Facet
- Fossa
- Fovea
- Groove
- Sulcus
- Canal
- Fissure
- Foramen
- Meatus
- Condyle
- Crest
- Epicondyle
- Head
- Line
- Protuberance
- Trochanter
- Tubercle
- Tuberosity
Part 6 – Review of terms and Definitions
- Define long bone, and give four examples
- Define short bone, and give four examples
- Define irregular bone, and give two examples
- Define flat bone, and give two examples
- Define sesamoid bone, and give an example
- A raised rough surface on a bone where a muscle attaches to is called?
- A round opening in a bone is called a .
- What are the components of the extracellular matrix of bone?
- What is the function of the osteoclasts?
- What is the difference between the distal and the proximal epiphysis?
Media Attributions
- Skeleton illustration © Wikipedia is licensed under a Public Domain license
- Compact Spongy bone © Wikipedia is licensed under a Public Domain license
- Compact bone histology © Wikipedia is licensed under a CC BY (Attribution) license
- Spongy bone trabecules © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Bone cells © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Classification of bones © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Long bone © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Anatomical Model of Bone © 3B Scientific is licensed under a All Rights Reserved license
- Label spongy bone © Maria Carles adapted by Michigan Medical School is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Label spongy bone zoom in © Maria Carles adapted by Michigan Medical School is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Label spongy bone structures © Maria Carles is licensed under a CC BY-SA (Attribution ShareAlike) license
- QR code V Microscope © Maria Carles is licensed under a CC BY-SA (Attribution ShareAlike) license
- Cartilage and bone © Maria Carles adapted by Michigan Medical School is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Label compact bone micrograph © Maria Carles adapted by Michigan Medical School is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Label compact bone high magnification © Wikipedia adapted by Michigan Medical School is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Longitudinal section of compact bone © Maria Carles adapted by Michigan Medical School is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Label shape of the bones © Maria Carles is licensed under a CC BY-SA (Attribution ShareAlike) license
- Structure of a Long Bone Label © Maria Carles is licensed under a CC BY-SA (Attribution ShareAlike) license
- Label flat bone © Maria Carles is licensed under a CC BY-SA (Attribution ShareAlike) license

