The Joints
Joints and Articulations Laboratory Activity
Objectives
- Define the term joint
- List the types of joints based on structure and give an example.
- List the names of joints based on structure and give an example.
- List and identify the structural components of a synovial joint.
- List types of synovial joints
- Identify the sutures of the skull.
- Identify the fontanelles.
- Identify the components of the knee joint.
- List type of movements in synovial joints.
Introduction
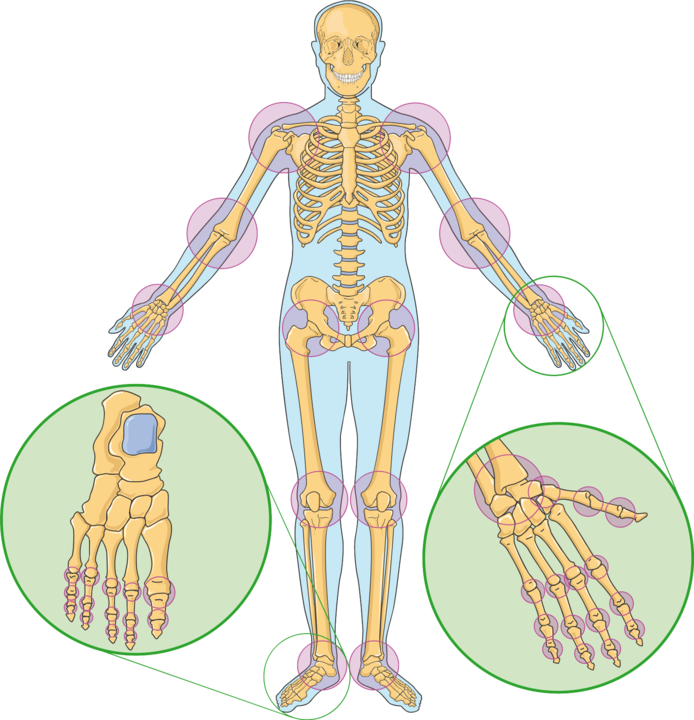
A joint or articulation is the connection made between 2 or more bones. They participate in degrees and types of movement. Joints may be classified based on function or structure.
Functional classification (movement)
Joints can also be classified functionally according to the type and degree of movement they allow: Joint movements are described with reference to the basic anatomical planes.
There are three types:
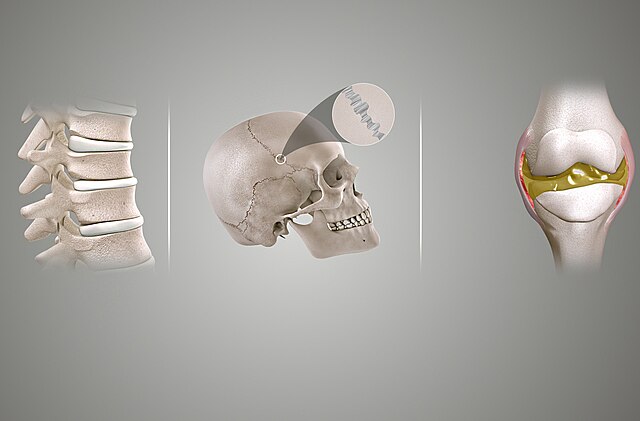
- Synarthrosis – permits no mobility. Most synarthrosis joints are fibrous joints (e.g. sutures of the skull).
- Amphiarthrosis – permits slight mobility. Most amphiarthrosis joints are cartilaginous joints (e.g., intervertebral discs).
- Diarthrosis – freely movable joints.
Structural classification names and divides joints according to the type of tissue that connects the bones to each other.
There are three structural classifications of joints:
- Fibrous joint: joined by dense regular connective tissue that is rich in collagen fibers.
- The subclasses of synarthrosis include:
- Sutures – periosteum of articulating bones interdigitate making a very stable joint, for example sutures of the skull
- Gomphosis – joint between the teeth and the alveolar process of the mandible or maxilla, it is held in place by the periodontal ligaments.
- Syndesmosis – located between two parallel articulating bones, they are joined by a long fibrous membrane called the interosseous membrane, these joints are classified as amphiarthrosis, for example the joint between the radius and the ulna.
- Cartilaginous joint: bones joined by cartilage or fibrocartilage. Most of this type of joint allows for some movement, so they are amphiarthrosis.
- There are two types of cartilaginous joints:
- Symphyses – bones are joint by a pad made of fibrocartilage (e.g. symphysis pubis)
- Synchondroses – bones joint by hyaline cartilage (e.g. costochondral joints)
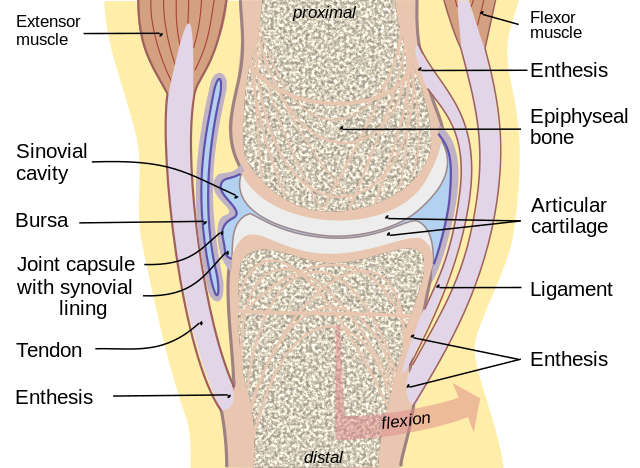
- Synovial joint: not directly joined, the bones have a synovial cavity filled with synovial fluid and are united by the dense irregular connective tissue that forms the articular capsule that is normally associated with accessory ligaments. They are diarthroses as they allow for free movement.
Synovial joints can in turn be classified into six groups according to the type of movement they allow:
- Plane joint – flat articular surfaces, allow for gliding movement.
- Ball and socket joint – where the convex of the end of one bone fits on the concave end of the other (e.g. shoulder joint).
- Hinge joint – a convex articular surface fits on the concave articular surface of the other, like a door hinge.
- Pivot joint – one bone rotates around another.
- Condyloid joint – one bone fits into the concave end of another (e.g. radiocarpal joint).
- Saddle joint – condyloid like but allow for more movement.
These are general terms that can be used to describe most movements the body makes. Most terms have a clear opposite, and so are treated in pairs.
Fontanelles
A fontanelle (or fontanel), colloquially known as soft spot, is an anatomical feature of the infant human skull comprising soft membranous gaps between the cranial bones that make up the calvaria of a fetus or an infant. Fontanelles allow for stretching and deformation of the neurocranium both during birth and later as the brain expands faster than the surrounding bone can grow.
The ossification of the bones of the skull causes the anterior fontanelle to close over by 9 to 18 months. The sphenoidal and posterior fontanelles close during the first few months of life. These closures eventually form the sutures of the neurocranium. Main fontanelles are the anterior and posterior fontanelles, the mastoid fontanelle and the sphenoidal fontanelle.
Premature complete ossification of the sutures is called craniosynostosis.
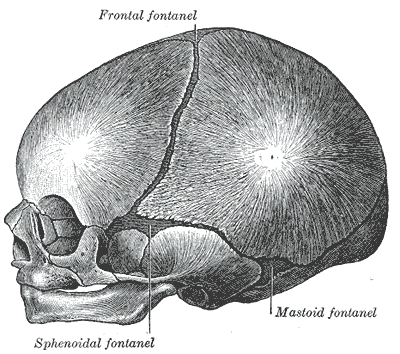
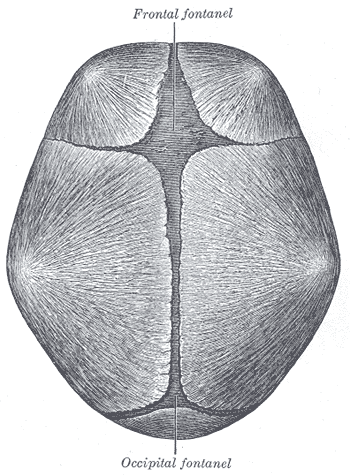
The skull at birth, showing the lateral fontanelles, anterior and posterior fontanelles
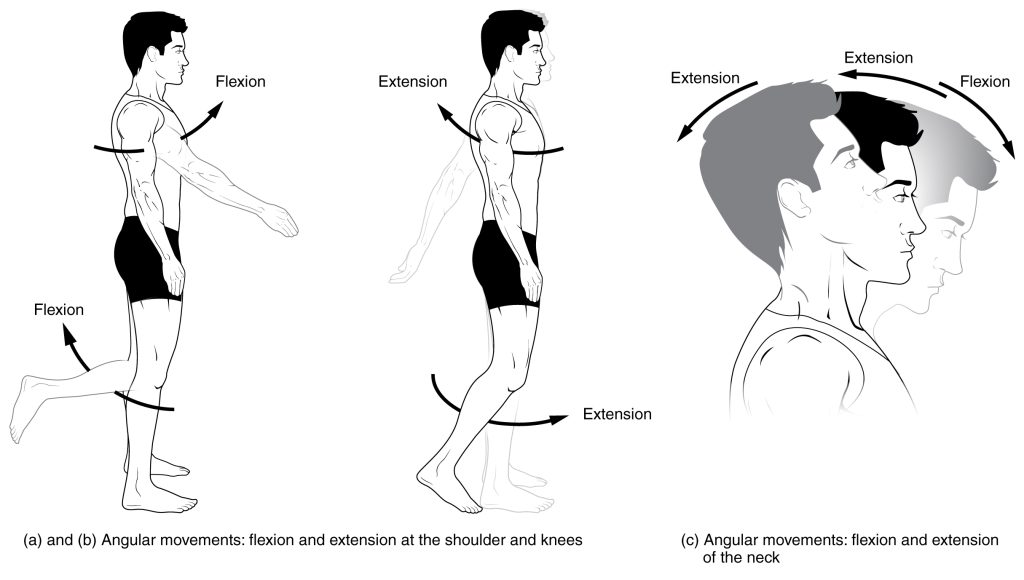
Types of Movements
Flexion and extension describe movements that affect the angle between two parts of the body. Flexion describes a bending movement that decreases the angle between a segment and its proximal segment. Extension is the opposite of flexion, describing a straightening movement that increases the angle between body parts
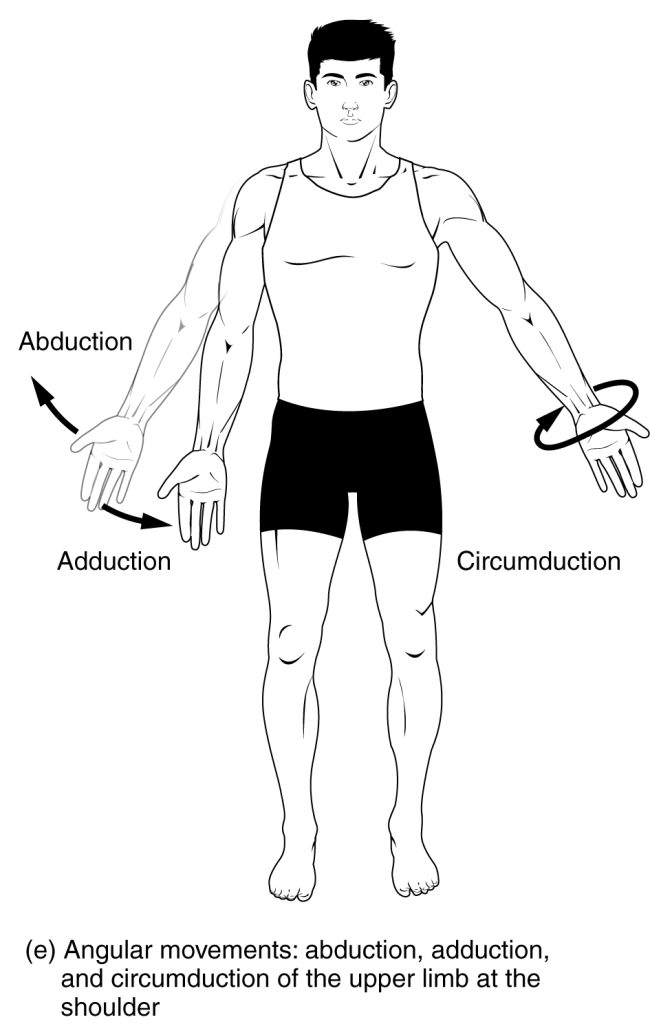
Abduction is the motion of a structure away from the midline while adduction refers to motion towards the center of the body. The center of the body is defined as the midsagittal plane. These terms come from Latin words with similar meanings, ab- being the Latin prefix indicating “away,” ad- indicating “toward,” and ducere meaning “to draw or pull” (cf. English words “duct,” “conduct,” “induction”). Abduction refers to a motion that pulls a structure or part away from the midline of the body. In the case of fingers and toes, it refers to spreading the digits apart, away from the centerline of the hand or foot. Adduction refers to a motion that pulls a structure or part toward the midline of the body, or towards the midline of a limb.
Circumduction refers to a conical movement of a body part, such as a ball and socket joint or the eye. Circumduction is a combination of flexion, extension, adduction and abduction. Circumduction can be best performed at ball and socket joints, such as the hip and shoulder, but may also be performed by other parts of the body such as fingers, hands, feet, and head.
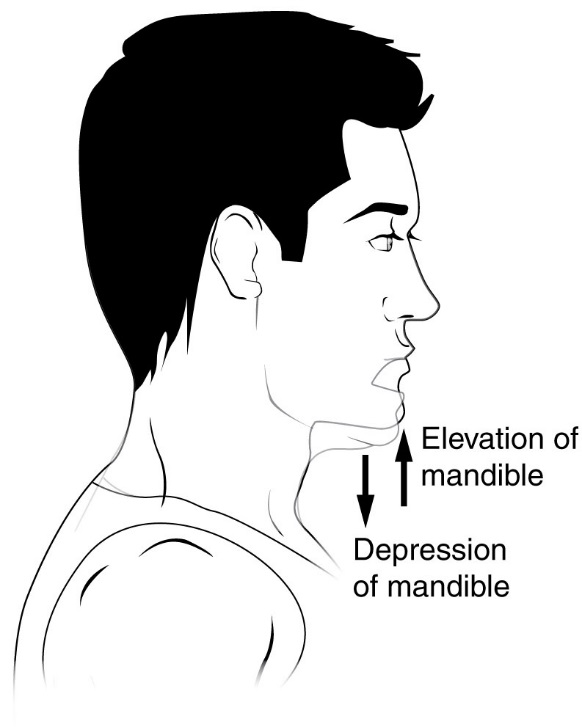
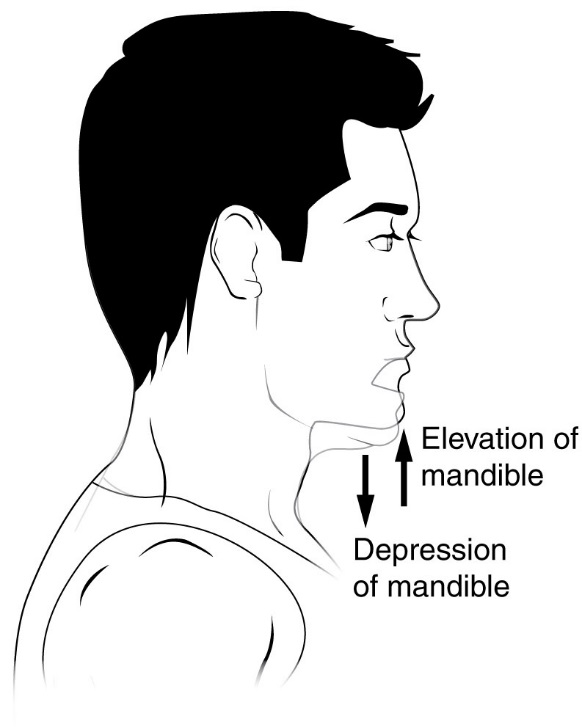
Elevation and depression
The terms elevation and depression refer to movement above and below the horizontal. Elevation refers to movement in a superior direction. Depression refers to movement in an inferior direction, the opposite of elevation.
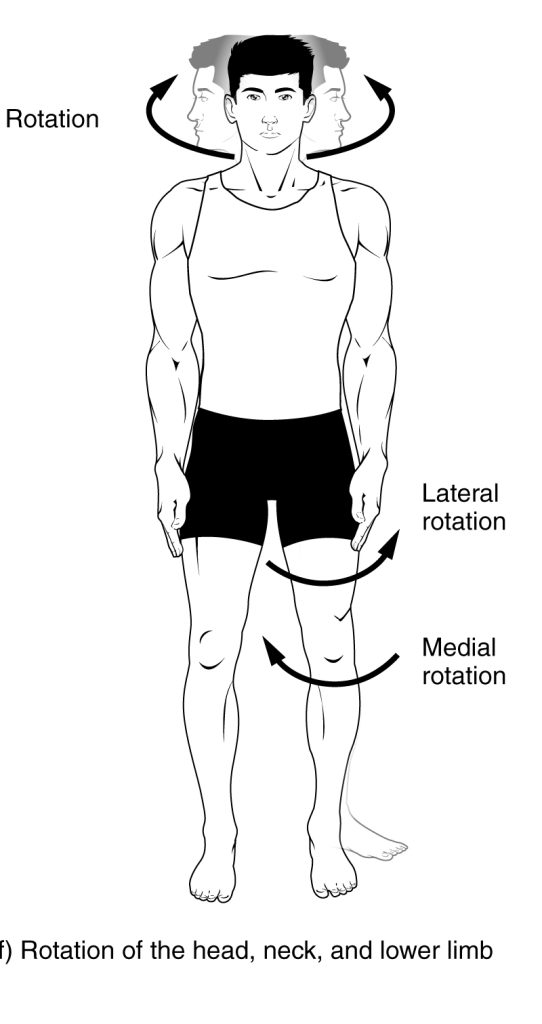
Rotation
Rotation of body parts is referred to as internal or external, referring to rotation towards or away from the center of the body. Internal rotation (or medial rotation) refers to rotation towards the axis of the body. External rotation (or lateral rotation) refers to rotation away from the center of the body.
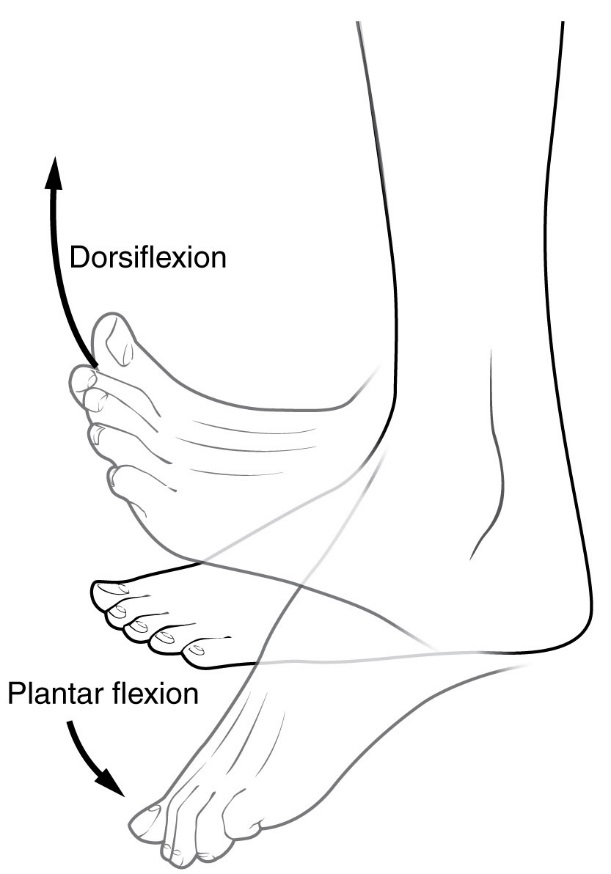
Dorsiflexion and plantar flexion refer to extension or flexion of the foot at the ankle. These terms refer to flexion in direction of the “back” of the foot, dorsum pedi, which is the upper surface of the foot when standing, and flexion in direction of the sole of the foot, plantar pedi. These terms are used to resolve confusion, as technically extension of the joint refers to dorsiflexion, which could be considered counter-intuitive as the motion reduces the angle between the foot and the leg. Dorsiflexion is where the toes are brought closer to the shin. This decreases the angle between the dorsum of the foot and the leg. Plantar flexion or plantarflexion is the movement which decreases the angle between the sole of the foot and the back of the leg.
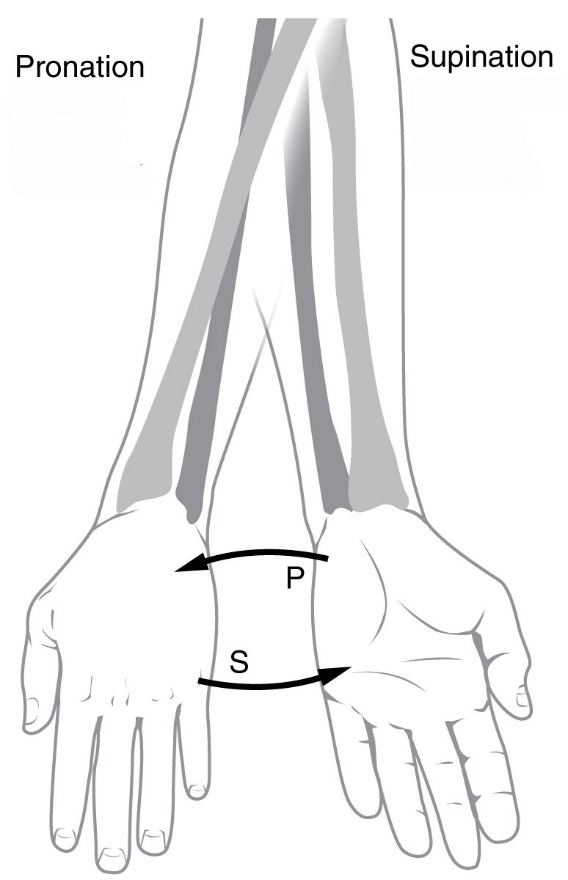
Pronation and supination refer most generally to assuming prone or supine positions, but often they are used in a specific sense referring to rotation of the forearm or foot so that in the standard anatomical position the palm or sole is facing anteriorly (supination) or posteriorly (pronation). Pronation at the forearm is a rotational movement where the hand and upper arm are turned inwards. Pronation of the foot refers to turning of the sole outwards, so that weight is borne on the medial part of the foot. Supination of the forearm occurs when the forearm or palm are rotated outwards. Supination of the foot refers to turning of the sole of the foot inwards, shifting weight to the lateral edge.
Inversion and eversion refer to movements that tilt the sole of the foot away from (eversion) or towards (inversion) the midline of the body. Eversion is the movement of the sole of the foot away from the median plane. Inversion is the movement of the sole towards the median plane.

Protrusion and retrusion are sometimes used to describe the anterior (protrusion) and posterior (retrusion) movement of the jaw.
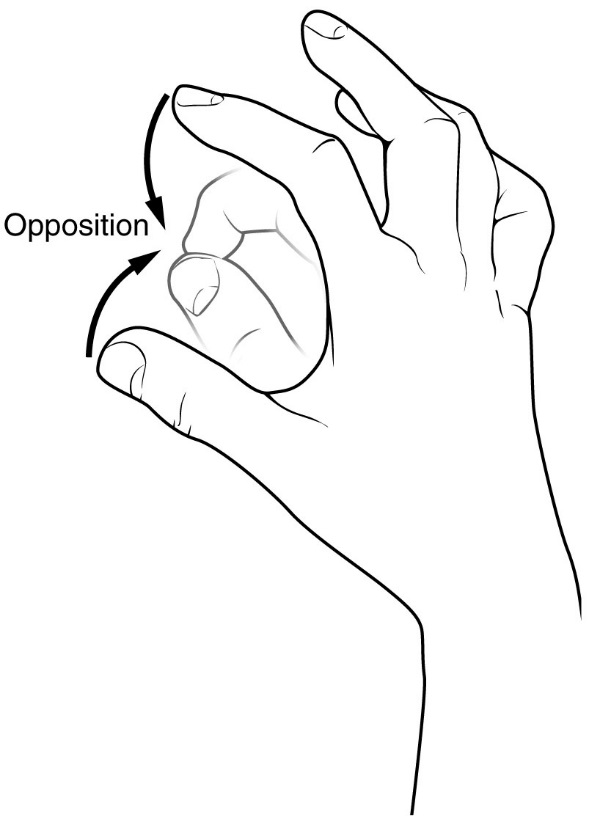
Opposition refers to the movement that involves grasping of the thumb and fingers. Reposition refers to restoring an object to its natural condition.
Protraction and Retraction refer to an anterior (protraction) or posterior (retraction) movement, such as of the arm at the shoulders, and the mandible.
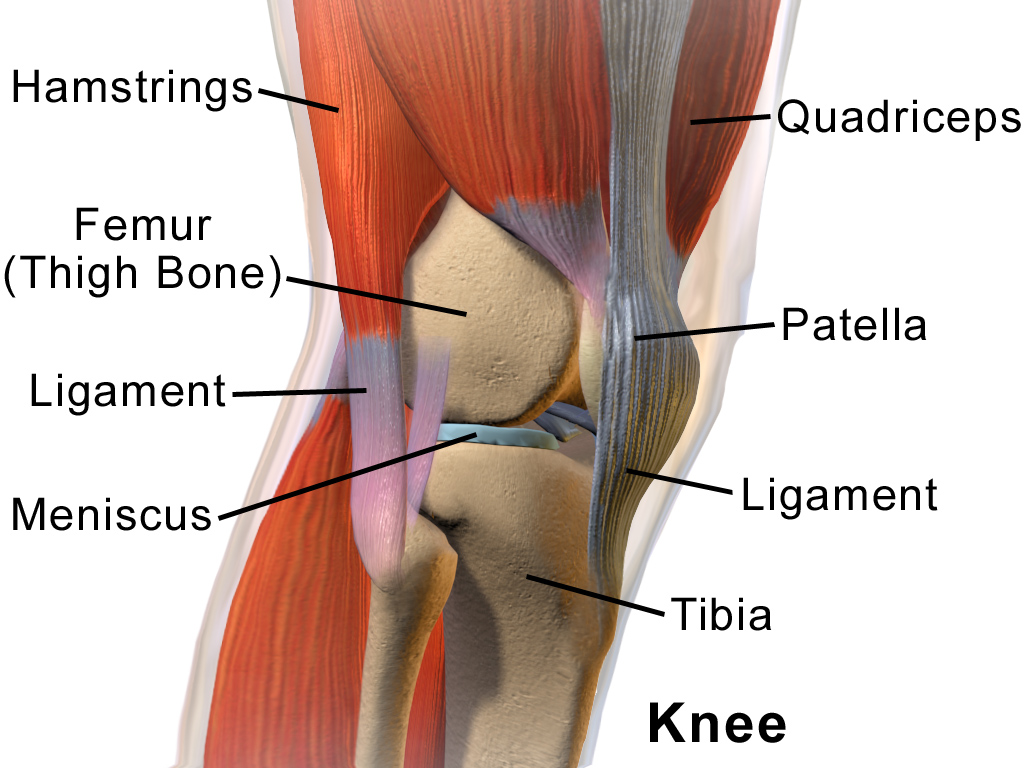
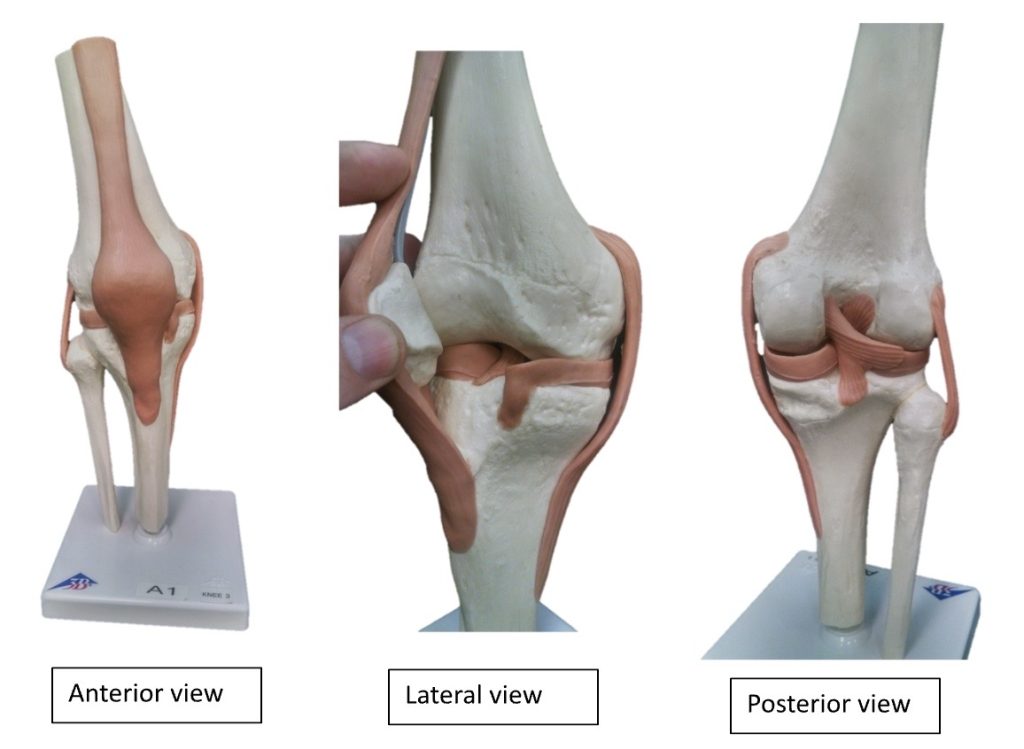
Lastly, we have selected one of the joints to study in detail for this lab activity, the Knee Joint. The other elbow, shoulder and hip joint will be shown superficially, make sure to pay attention to the structures that compose the knee joint, it is the most complex of all of them and it will give you a good idea of how a synovial joint functions.
The knee joins the thigh with the leg and consists of two joints: tibiofemoral joint (between femur and tibia), and patellofemoral joint (between femur and patella). It is the largest joint in the human body.
The knee is a modified hinge joint, which permits flexion and extension as well as slight internal and external rotation. The joint is bathed in synovial fluid which is contained inside the synovial membrane called the joint capsule.
The articular bodies of the knee joint include the articular bodies of the femur (lateral and medial condyles), a pair of tibial condyles are separated by the intercondylar eminence and the patella.
The articular capsule has a synovial and a fibrous membrane separated by fatty deposits. Anteriorly, the synovial membrane is attached on the margin of the cartilage both on the femur and the tibia, but on the femur, the suprapatellar bursa or recess extends the joint space proximally. The suprapatellar bursa is prevented from being pinched during extension by the Articularis genus muscle. Behind, the synovial membrane is attached to the margins of the two femoral condyles which produces two extensions similar to the anterior recess. Between these two extensions, the synovial membrane passes in front of the two cruciate ligaments at the center of the joint, thus forming a pocket directly inward.
There are numerous bursae surround the knee joint. The largest communicative bursa is the suprapatellar bursa described above. Four considerably smaller bursae are located on the back of the knee. Two non-communicative bursae are located in front of the patella and below the patellar tendon, and others are sometimes present.
The cartilage ensures supple knee movement. There are two types of joint cartilage in the knees: fibrous cartilage (the meniscus) and hyaline cartilage. Fibrous cartilage has tensile strength and can resist pressure. Hyaline cartilage covers the surface along which the joints move. There are no blood vessels inside of the hyaline cartilage, the alimentation is performed per diffusion. Synovial fluid and the subchondral bone marrow serve both as nutrition sources for the hyaline cartilage. Lack of at least one source induces a degeneration. Cartilage will wear over the years. Cartilage has a very limited capacity for self-restoration. The newly formed tissue will generally consist of a large part of fibrous cartilage of lesser quality than the original hyaline cartilage. As a result, new cracks and tears will form in the cartilage over time.
The articular discs of the knee-joint are called menisci because they only partly divide the joint space. These two disks, the medial meniscus and the lateral meniscus, consist of connective tissue with extensive collagen fibers containing cartilage-like cells. The menisci are flattened at the center of the knee joint, fused with the synovial membrane laterally, and can move over the tibial surface. The menisci serve to protect the ends of the bones from rubbing on each other and to effectively deepen the tibial sockets into which the femur attaches. They also play a role in shock absorption, and may be cracked, or torn, when the knee is forcefully rotated and/or bent.
The ligaments surrounding the knee joint offer stability by limiting movements and, together with the menisci and several bursae, protect the articular capsule.
There are two types of ligaments in the knee joint, the intracapsular and extracapsular ligaments. The intracapsular ligaments include a pair of cruciate ligaments, transverse ligament, meniscofemoral ligaments, and the menisco-tibial ligaments that stabilize the knee.
The anterior cruciate ligament (ACL) stretches from the lateral condyle of femur to the anterior intercondylar area. The ACL is critically important because it prevents the tibia from being pushed too far anterior relative to the femur. It is often torn during twisting or bending of the knee. The posterior cruciate ligament (PCL) stretches from the medial condyle of femur to the posterior intercondylar area. Injury to this ligament is uncommon but can occur as a direct result of forced trauma to the ligament. This ligament prevents posterior displacement of the tibia relative to the femur. The transverse ligament stretches from the lateral meniscus to the medial meniscus. It passes in front of the menisci. The two menisci are attached to each other anteriorly by the ligament. The posterior and anterior meniscofemoral ligaments stretch from the posterior horn of the lateral meniscus to the medial femoral condyle. They pass posteriorly behind the posterior cruciate ligament. The posterior meniscofemoral ligament is more commonly present (30%); both ligaments are present less often. The menisco-tibial ligaments (or “coronary”) stretches from inferior edges of the mensici to the periphery of the tibial plateaus. The extracapsular ligaments include the patellar ligament, medial and lateral collateral ligaments, oblique popliteal ligament and arcuate popliteal ligament.
The patellar ligament connects the patella to the tuberosity of the tibia. It is also occasionally called the patellar tendon because there is no definite separation between the quadriceps tendon (which surrounds the patella) and the area connecting the patella to the tibia, it mat be more appropriate even though there is no physical division between the two, to call the upper portion the rectus femoris tendon and the lower portion the patellar ligament. This very strong ligament helps give the patella its mechanical leverage and also functions as a cap for the condyles of the femur. Laterally and medially to the patellar ligament the lateral and medial retinacula connect fibers from the vasti lateralis and medialis muscles to the tibia. Some fibers from the iliotibial tract radiate into the lateral retinaculum and the medial retinaculum receives some transverse fibers arising on the medial femoral epicondyle. The medial collateral ligament (MCL a.k.a. “tibial”) stretches from the medial epicondyle of the femur to the medial tibial condyle. It is composed of three groups of fibers, one stretching between the two bones, and two fused with the medial meniscus. The MCL is partly covered by the pes anserinus and the tendon of the semimembranosus passes under it. It protects the medial side of the knee from being bent open by a stress applied to the lateral side of the knee (a valgus force). The fibular collateral ligament (LCL a.k.a. “fibular”) stretches from the lateral epicondyle of the femur to the head of fibula. It is separate from both the joint capsule and the lateral meniscus. It protects the lateral side from an inside bending force. Lastly, there are two ligaments on the dorsal side of the knee. The oblique popliteal ligament is a radiation of the tendon of the semimembranosus on the medial side, from where it is direct laterally and proximally. The arcuate popliteal ligament originates on the apex of the head of the fibula to stretch proximally, crosses the tendon of the popliteus muscle, and passes into the capsule.
Note: On the anatomical model of the knee we have in the lab, we can’t identify all of the intra and extracapsular ligaments, they usually a few of them only.
Anterolateral and anteromedial aspects of the knee
Laboratory activity
- Classification of JointsProcedureProcedure
-
- Classify joints by structure and function. Inspect the anatomical models your instructor placed on the lab bench. Classify the joints by structure and function. You may also add the structural subcategory and the amount of motion that the joint allows to your answers. Write your answers in the table provided below.
Table No. 1 – Classification of Joints
| Joint | Structural classification | Functional classification |
| Atlantoaxial joint | ||
| Atlantooccipital joint | ||
| Coronal suture | ||
| Costochondral joint | ||
| Glenohumeral joint (shoulder) | ||
| Intervertebral joint | ||
| Knee joint | ||
| Radioulnar joint | ||
| Sagittal suture | ||
| Tibiofibular joint | ||
| Tooth joint |
- Identify the structures of a synovial joint.

- Identify structures of the knee joint.
Procedure
Using the Anatomical model of the knee and the diagrams shown above, identify the following structures:
Table No. 2 – Structures of the knee
| Structure | Identified (✓/X) |
| Anterior cruciate ligament (ACL) | |
| Articular surface of the femur | |
| Bursae | |
| Femur | |
| Joint capsule | |
| Lateral collateral ligament | |
| Lateral condyle of femur | |
| Lateral meniscus | |
| Medial collateral ligament | |
| Medial condyle of femur | |
| Medial meniscus | |
| Patella | |
| Patellar ligament | |
| Posterior cruciate ligament (PCL) | |
| Quadriceps muscle | |
| Synovial cavity (with synovial fluid) | |
| Synovial membrane | |
| Tendon of the rectus femoris | |
| Tibia |
- Label the structures of the knee using the knee anatomical model (for 100% online, use the images provided here).
- Using the anatomical model of a newborn skull, label the main fontanelles, anterior, posterior, sphenoid and mastoid fontanelles. For 100% online courses, use the image provided here.

Motions of Synovial Joints
Define the following terms using the table provided here:
Table No. 3 – Definitions
| Movement | Definition |
| Abduction | |
| Adduction | |
| Circumduction | |
| Depression | |
| Dorsiflexion | |
| Eversion | |
| Elevation | |
| Extension | |
| Flexion | |
| Inversion | |
| Opposition | |
| Plantar flexion | |
| Protraction | |
| Retraction | |
| Rotation | |
| Supination |
- Determine the type of Movement at synovial joints
Using the images shown below, determine the type of movement shown. Write your answers on the table provided below.
Movements
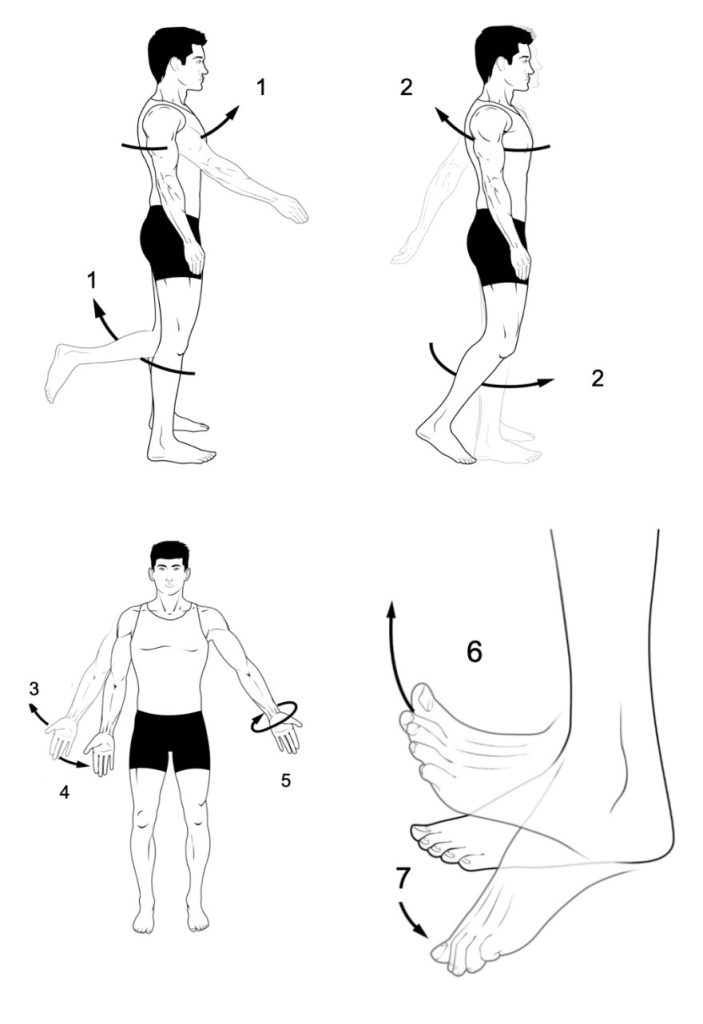
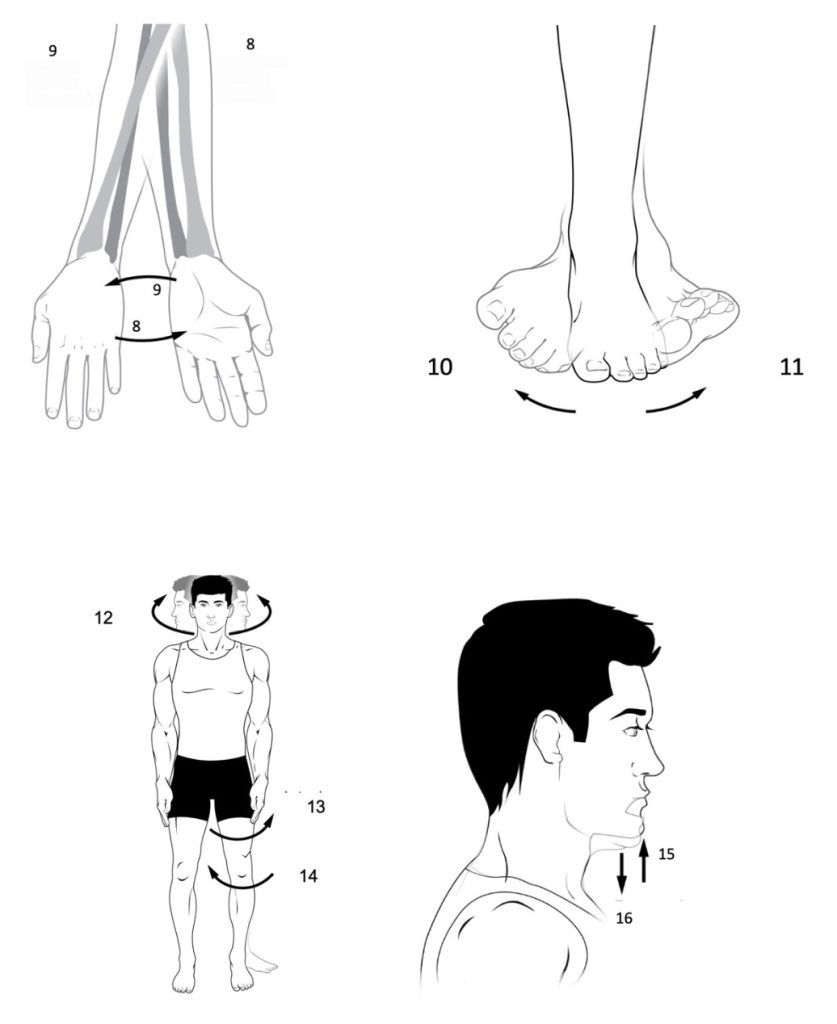
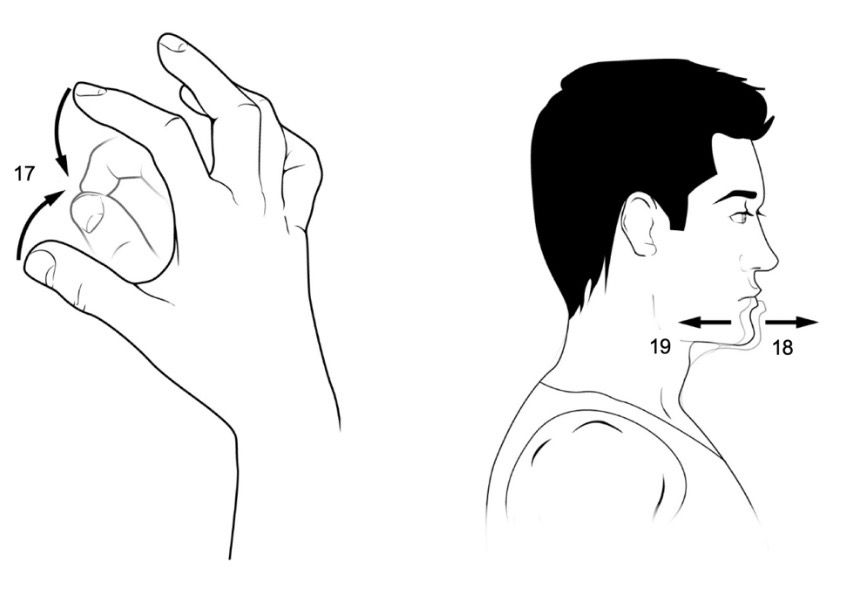
Table No. 4 – Types of Movement
| Figure # | Type of movement |
| 1 | |
| 2 | |
| 3 | |
| 4 | |
| 5 | |
| 6 | |
| 7 | |
| 8 | |
| 9 | |
| 10 | |
| 11 | |
| 12 | |
| 13 | |
| 14 | |
| 15 | |
| 16 | |
| 17 | |
| 18 |
Word bank: Abduction, Adduction, Circumduction, Depression, Dorsiflexion, Eversion, Elevation, Extension, Flexion, Inversion, Opposition, Plantar flexion, Protraction, Retraction, Rotation, Rotation (lateral), Rotation (medial), Supination.
Review the Following Structures:
Sutures
Coronal
Sagittal
Lambdoidal
Squamous suture
Fontanelles
Anterior fontanelle
Posterior fontanelle
Anterolateral fontanelle (sphenoidal)
Posterolateral fontanelle (mastoid)
Syndesmoses
Radioulnar joint
Tibiofibular joint
Gomphoses
Synchondroses
Sternocostal
Symphysis
Symphysis pubis
Synovial joints
Bursa
Articular Capsule
Fibrous capsule
Synovial membrane
Synovial cavity
Knee Joint
Femur
Medial condyle + Articular cartilage
Lateral condyle + Articular cartilage
ACL, Anterior cruciate ligament
PCL, Posterior cruciate ligament
Lateral collateral ligament
Medial collateral ligament
Lateral meniscus
Medial meniscus
Tibia
Medial Condyle + Articular cartilage
Lateral Condyle + Articular cartilage
Patella
Patellar ligament
Tendon of quadriceps femoris
Media Attributions
- Joints © By Laboratoires Servier - Smart Servier website: Images related to Joints, Skeleton and bones and Bones -- Download in Powerpoint format.Flickr: Images related to Joints, Skeleton and bones and Bones (in French)., CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=82641187 is licensed under a CC BY-SA (Attribution ShareAlike) license
- Structural classification of joints © By www.scientificanimations.com - http://www.scientificanimations.com/wiki-images/, CC BY-SA 4.0, https://commons.wikimedia.org/w/index.php?curid=74552215 is licensed under a CC BY-SA (Attribution ShareAlike) license
- Joint © By Madhero88 - Own work, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=10158699 is licensed under a CC BY-SA (Attribution ShareAlike) license
- Frontal © By Henry Vandyke Carter - Henry Gray (1918) Anatomy of the Human Body (See "Book" section below)Bartleby.com: Gray's Anatomy, Plate 198, Public Domain, https://commons.wikimedia.org/w/index.php?curid=792102 is licensed under a Public Domain license
- Frontal 2 © By Henry Vandyke Carter - Henry Gray (1918) Anatomy of the Human Body (See "Book" section below)Bartleby.com: Gray's Anatomy, Plate 198, Public Domain, https://commons.wikimedia.org/w/index.php?curid=792102 is licensed under a CC BY-SA (Attribution ShareAlike) license
- Flexsion Extension © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Body movements © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Elevation and Depression © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Body movements rotation © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Dorsiplantar © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Pronation and supination © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Eversion and inversion © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Opposition © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Knee Anatomy Side © By BruceBlaus. When using this image in external sources it can be cited as:Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. - Own work, CC BY 3.0, https://commons.wikimedia.org/w/index.php?curid=29987037 is licensed under a CC BY-SA (Attribution ShareAlike) license
- Knee diagram © By Mysid - Vectorized and colorized in Inkscape, based on Image:Knee diagram.png., Public Domain, https://commons.wikimedia.org/w/index.php?curid=4004042 is licensed under a CC BY-SA (Attribution ShareAlike) license
- Knee medial view © Wikipedia is licensed under a Public Domain license
- synovial joint © Maria Carles is licensed under a CC BY-SA (Attribution ShareAlike) license
- Knee labeled anatomical models © Maria Carles is licensed under a CC BY-SA (Attribution ShareAlike) license
- Fontanelle © Wikipedia is licensed under a Public Domain license
- Movements label 1 © Maria Carles adapted by Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Movements label 2 © Maria Carles adapted by Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Movements label 3 © Maria Carles adapted by Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license