The Nervous System Anatomy
The Brain and Cranial Nerves
Objectives
- Identify the three meninges that cover the brain.
- Identify the major regions of the brain and the basic function of each region.
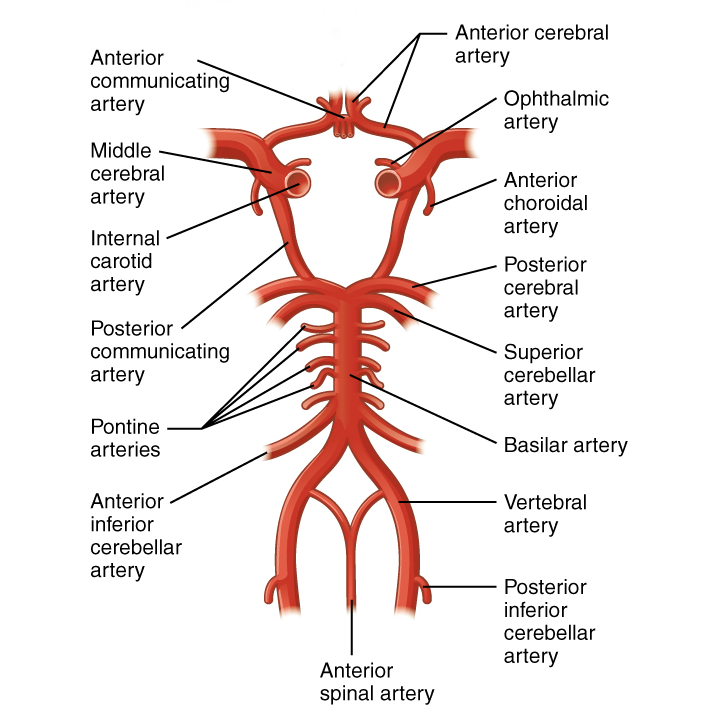
- Describe the vessels that supply the CNS.
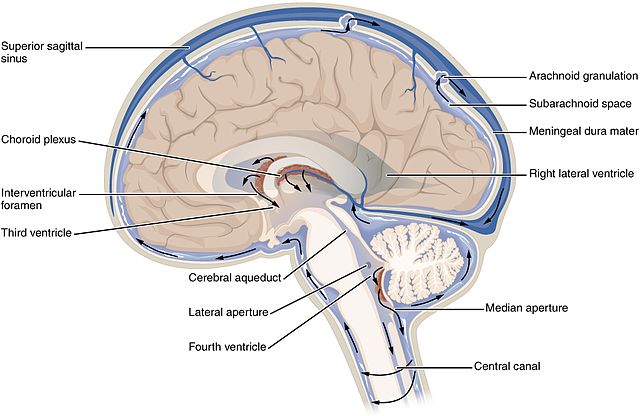
- Name the components of the ventricular system and the regions of the brain in which each is located.
- Explain the production of cerebrospinal fluid and its flow through the ventricles.
- Identify and describe the function of the cranial nerves.
The Central Nervous System (CNS) is composed of the brain and the spinal cord. The adult brain has two hemispheres attached by a structure called the corpus callosum and it is further described by four major regions: the cerebrum, the diencephalon, the brainstem, and the cerebellum. As the brain extends posteriorly and passes through the foramen magnum becomes the spinal cord.
Regulation of homeostasis is governed by two systems: namely, the Nervous system and the Endocrine system. They work in association to coordinate all functions of our organ systems. The nervous system sends electrical signals (action potentials) between cells and the endocrine system chemical signals (hormones) via the circulatory system.
Let’s describe the regions of the brain and its functions.
The Cerebrum
The iconic gray mantle of the human brain, which appears to make up most of the mass of the brain, is the cerebrum. The wrinkled portion is the cerebral cortex, and the rest of the structure is beneath that outer covering. There is a large separation between the two sides of the cerebrum called the longitudinal fissure. It separates the cerebrum into two distinct halves, a right and left cerebral hemisphere. Deep within the cerebrum, the white matter of the corpus callosum provides the major pathway for communication between the two hemispheres of the cerebral cortex.
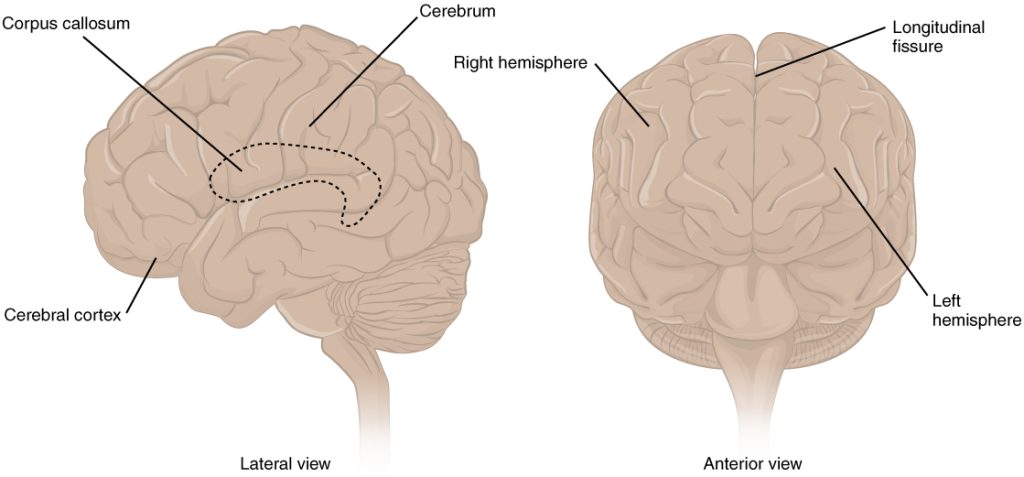
Many of the higher neurological functions, such as memory, emotion, and consciousness, are the result of cerebral function. The complexity of the cerebrum is different across vertebrate species. The cerebrum of the most primitive vertebrates is not much more than the connection for the sense of smell. In mammals, the cerebrum comprises the outer gray matter that is the cortex (from the Latin word meaning “bark of a tree”) and several deep nuclei that belong to three important functional groups. The basal nuclei are responsible for cognitive processing, the most important function being that associated with planning movements. The basal forebrain contains nuclei that are important in learning and memory. The limbic cortex is the region of the cerebral cortex that is part of the limbic system, a collection of structures involved in emotion, memory, and behavior.
Cerebral Cortex
The cerebrum is covered by a continuous layer of gray matter that wraps around either side of the forebrain—the cerebral cortex. This thin, extensive region of wrinkled gray matter is responsible for the higher functions of the nervous system. A gyrus (plural = gyri) is the ridge of one of those wrinkles, and a sulcus (plural = sulci) is the groove between two gyri. The pattern of these folds of tissue indicates specific regions of the cerebral cortex.
The head is limited by the size of the birth canal, and the brain must fit inside the cranial cavity of the skull. Extensive folding in the cerebral cortex enables more gray matter to fit into this limited space. If the gray matter of the cortex were peeled off of the cerebrum and laid out flat, its surface area would be roughly equal to one square meter.
The folding of the cortex maximizes the amount of gray matter in the cranial cavity. During embryonic development, as the telencephalon expands within the skull, the brain goes through a regular course of growth that results in everyone’s brain having a similar pattern of folds. The surface of the brain can be mapped on the basis of the locations of large gyri and sulci. Using these landmarks, the cortex can be separated into four major regions, or lobes. The lateral sulcus that separates the temporal lobe from the other regions is one such landmark. Superior to the lateral sulcus are the parietal lobe and frontal lobe, which are separated from each other by the central sulcus. The posterior region of the cortex is the occipital lobe, which has no obvious anatomical border between it and the parietal or temporal lobes on the lateral surface of the brain. From the medial surface, an obvious landmark separating the parietal and occipital lobes is called the parieto-occipital sulcus. The fact that there is no obvious anatomical border between these lobes is consistent with the functions of these regions being interrelated.
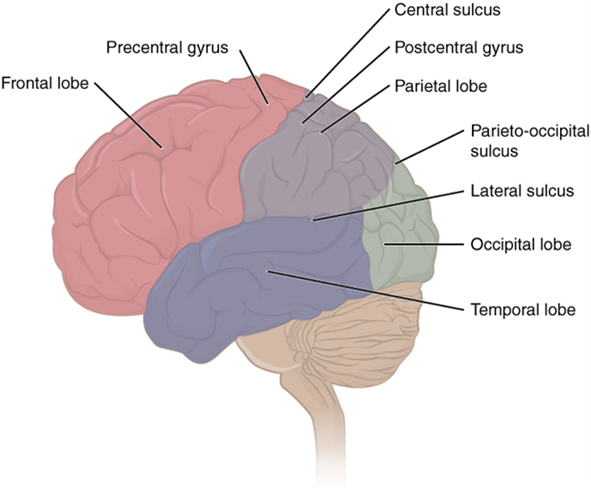
Different regions of the cerebral cortex can be associated with particular functions, a concept known as localization of function. In the early 1900s, a German neuroscientist named Korbinian Brodmann performed an extensive study of the microscopic anatomy—the cytoarchitecture—of the cerebral cortex and divided the cortex into 52 separate regions on the basis of the histology of the cortex. His work resulted in a system of classification known as Brodmann’s areas, which is still used today to describe the anatomical distinctions within the cortex. The results from Brodmann’s work on the anatomy align very well with the functional differences within the cortex. Areas 17 and 18 in the occipital lobe are responsible for primary visual perception. That visual information is complex, so it is processed in the temporal and parietal lobes as well.
The temporal lobe is associated with primary auditory sensation, known as Brodmann’s areas 41 and 42 in the superior temporal lobe. Because regions of the temporal lobe are part of the limbic system, memory is an important function associated with that lobe. Memory is essentially a sensory function; memories are recalled sensations such as the smell of Mom’s baking or the sound of a barking dog. Even memories of movement are really the memory of sensory feedback from those movements, such as stretching muscles or the movement of the skin around a joint. Structures in the temporal lobe are responsible for establishing long-term memory, but the ultimate location of those memories is usually in the region in which the sensory perception was processed.
The main sensation associated with the parietal lobe is somatosensation, meaning the general sensations associated with the body. Posterior to the central sulcus is the postcentral gyrus, the primary somatosensory cortex, which is identified as Brodmann’s areas 1, 2, and 3. All of the tactile senses are processed in this area, including touch, pressure, tickle, pain, itch, and vibration, as well as more general senses of the body such as proprioception and kinesthesia, which are the senses of body position and movement, respectively.
Anterior to the central sulcus is the frontal lobe, which is primarily associated with motor functions. The precentral gyrus is the primary motor cortex. Cells from this region of the cerebral cortex are the upper motor neurons that instruct cells in the spinal cord and brainstem (lower motor neurons) to move skeletal muscles. Anterior to this region are a few areas that are associated with planned movements. The premotor area is responsible for storing learned movement algorithms which are instructions for complex movements. Different algorithms activate the upper motor neurons in the correct sequence when a complex motor activity is performed. The frontal eye fields are important in eliciting scanning eye movements and in attending to visual stimuli. Broca’s area is responsible for the production of language, or controlling movements responsible for speech; in the vast majority of people, it is located only on the left side. Anterior to these regions is the prefrontal lobe, which serves cognitive functions that can be the basis of personality, short-term memory, and consciousness. The prefrontal lobotomy is an outdated mode of treatment for personality disorders (psychiatric conditions) that profoundly affected the personality of the patient.
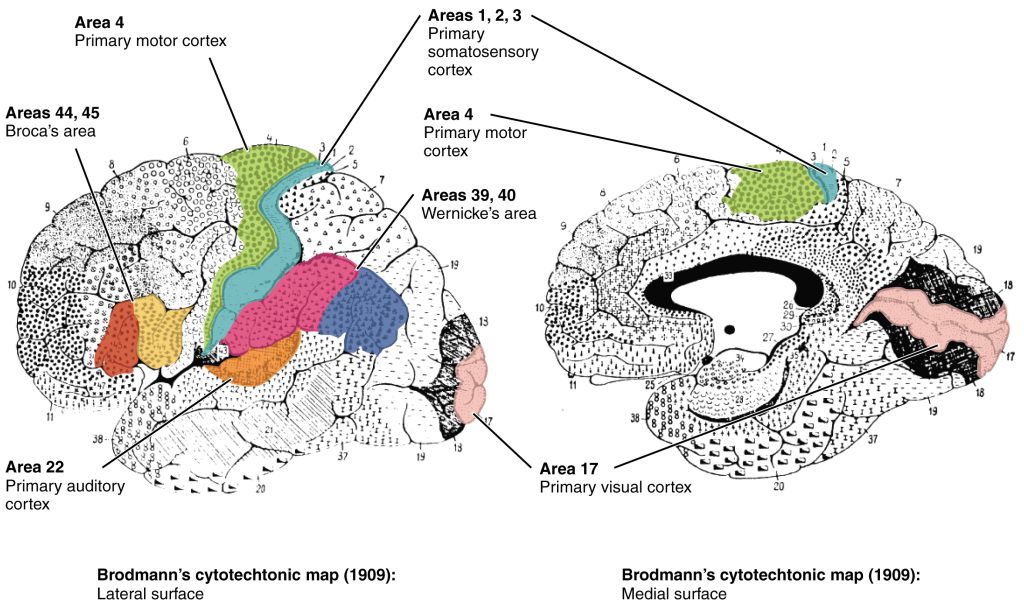
Area 17, as Brodmann described it, is also known as the primary visual cortex. Adjacent to that are areas 18 and 19, which constitute subsequent regions of visual processing. Area 22 is the primary auditory cortex, and it is followed by area 23, which further processes auditory information. Area 4 is the primary motor cortex in the precentral gyrus, whereas area 6 is the premotor cortex. These areas suggest some specialization within the cortex for functional processing, both in sensory and motor regions. The fact that Brodmann’s areas correlate so closely to functional localization in the cerebral cortex demonstrates the strong link between structure and function in these regions.
Areas 1, 2, 3, 4, 17, and 22 are each described as primary cortical areas. The adjoining regions are each referred to as association areas. Primary areas are where sensory information is initially received from the thalamus for conscious perception, or—in the case of the primary motor cortex—where descending commands are sent down to the brainstem or spinal cord to execute movements.
Functions of the Cerebral Cortex
The cerebrum is the seat of many of the higher mental functions, such as memory and learning, language, and conscious perception, which are the subjects of subtests of the mental status exam. The cerebral cortex is the thin layer of gray matter on the outside of the cerebrum. It is approximately a millimeter thick in most regions and highly folded to fit within the limited space of the cranial vault. These higher functions are distributed across various regions of the cortex, and specific locations can be said to be responsible for particular functions. There is a limited set of regions, for example, that are involved in language function, and they can be subdivided on the basis of the particular part of language function that each governs.
A number of other regions, which extend beyond these primary or association areas of the cortex, are referred to as integrative areas. These areas are found in the spaces between the domains for particular sensory or motor functions, and they integrate multisensory information, or process sensory or motor information in more complex ways. Consider, for example, the posterior parietal cortex that lies between the somatosensory cortex and visual cortex regions. This has been ascribed to the coordination of visual and motor functions, such as reaching to pick up a glass. The somatosensory function that would be part of this is the proprioceptive feedback from moving the arm and hand. The weight of the glass, based on what it contains, will influence how those movements are executed.

Blood Supply to the Brain
A lack of oxygen to the CNS can be devastating, and the cardiovascular system has specific regulatory reflexes to ensure that the blood supply is not interrupted. There are multiple routes for blood to get into the CNS, with specializations to protect that blood supply and to maximize the ability of the brain to get an uninterrupted perfusion.
Arterial Supply
The major artery carrying recently oxygenated blood away from the heart is the aorta. The very first branches off the aorta supply the heart with nutrients and oxygen. The next branches give rise to the common carotid arteries, which further branch into the internal carotid arteries. The external carotid arteries supply blood to the tissues on the surface of the cranium. The bases of the common carotids contain stretch receptors that immediately respond to the drop in blood pressure upon standing. The orthostatic reflex is a reaction to this change in body position, so that blood pressure is maintained against the increasing effect of gravity (orthostatic means “standing up”). Heart rate increases—a reflex of the sympathetic division of the autonomic nervous system—and this raises blood pressure.
The internal carotid artery enters the cranium through the carotid canal in the temporal bone. A second set of vessels that supply the CNS are the vertebral arteries, which are protected as they pass through the neck region by the transverse foramina of the cervical vertebrae. The vertebral arteries enter the cranium through the foramen magnum of the occipital bone. Branches off the left and right vertebral arteries merge into the anterior spinal artery supplying the anterior aspect of the spinal cord, found along the anterior median fissure. The two vertebral arteries then merge into the basilar artery, which gives rise to branches to the brainstem and cerebellum. The left and right internal carotid arteries and branches of the basilar artery all become the circle of Willis, a confluence of arteries that can maintain perfusion of the brain even if narrowing or a blockage limits flow through one part.
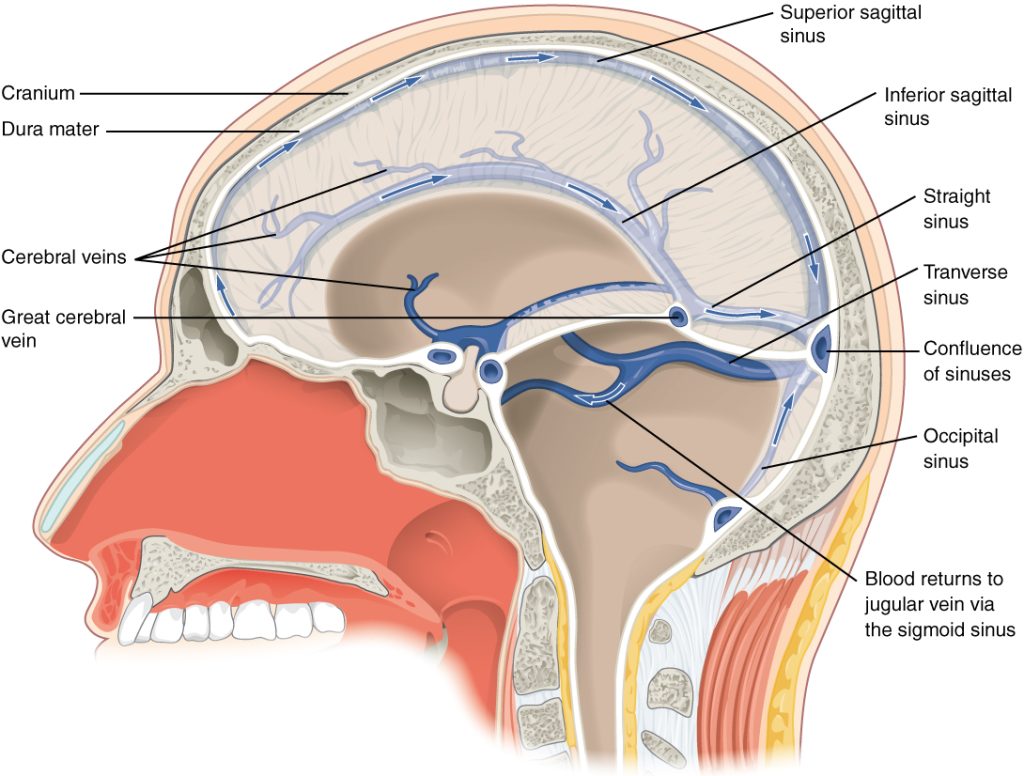
Venous Return
After passing through the CNS, blood returns to the circulation through a series of dural sinuses and veins. The superior sagittal sinus runs in the groove of the longitudinal fissure, where it absorbs CSF from the meninges. The superior sagittal sinus drains to the confluence of sinuses, along with the occipital sinuses and straight sinus, to then drain into the transverse sinuses. The transverse sinuses connect to the sigmoid sinuses, which then connect to the jugular veins. From there, the blood continues toward the heart to be pumped to the lungs for reoxygenation.
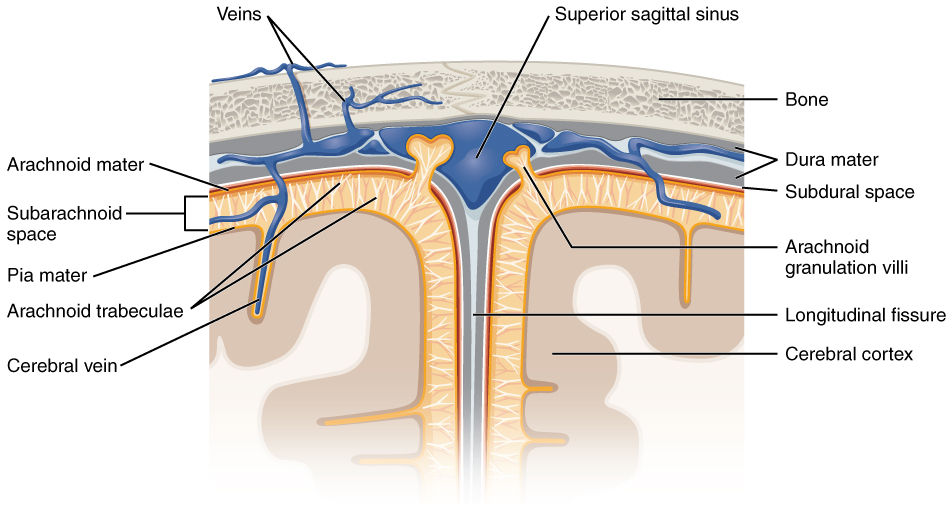
Protective Coverings of the Brain and Spinal Cord
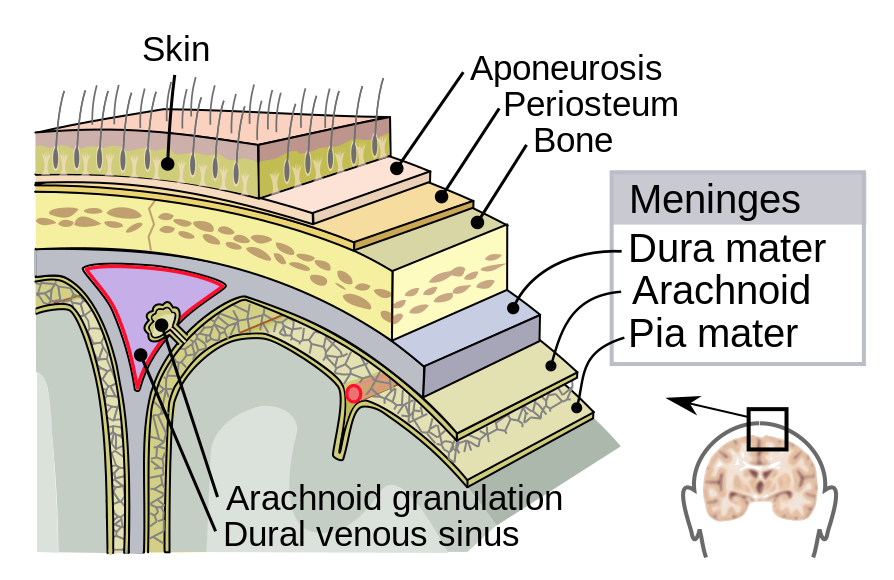
The outer surface of the CNS is covered by a series of membranes composed of connective tissue called the meninges, which protect the brain. The dura mater is a thick fibrous layer and a strong protective sheath over the entire brain and spinal cord. It is anchored to the inner surface of the cranium and vertebral cavity. The arachnoid mater is a membrane of thin fibrous tissue that forms a loose sac around the CNS. Beneath the arachnoid is a thin, filamentous mesh called the arachnoid trabeculae, which looks like a spider web, giving this layer its name. Directly adjacent to the surface of the CNS is the pia mater, a thin fibrous membrane that follows the convolutions of gyri and sulci in the cerebral cortex and fits into other grooves and indentations.
Dura Mater
Like a thick cap covering the brain, the dura mater is a tough outer covering. The name comes from the Latin for “tough mother” to represent its physically protective role. It encloses the entire CNS and the major blood vessels that enter the cranium and vertebral cavity. It is directly attached to the inner surface of the bones of the cranium and to the very end of the vertebral cavity.
There are infoldings of the dura that fit into large crevasses of the brain. Two infoldings go through the midline separations of the cerebrum and cerebellum; one forms a shelf-like tent between the occipital lobes of the cerebrum and the cerebellum, and the other surrounds the pituitary gland. The dura also surrounds and supports the venous sinuses.
Arachnoid Mater
The middle layer of the meninges is the arachnoid, named for the spider-web–like trabeculae between it and the pia mater. The arachnoid defines a sac-like enclosure around the CNS. The trabeculae are found in the subarachnoid space, which is filled with circulating CSF. The arachnoid emerges into the dural sinuses as the arachnoid granulations, where the CSF is filtered back into the blood for drainage from the nervous system.
The subarachnoid space is filled with circulating CSF, which also provides a liquid cushion to the brain and spinal cord. Similar to clinical blood work, a sample of CSF can be withdrawn to find chemical evidence of neuropathology or metabolic traces of the biochemical functions of nervous tissue.
Pia Mater
The outer surface of the CNS is covered in the thin fibrous membrane of the pia mater. It is thought to have a continuous layer of cells providing a fluid-impermeable membrane. The name pia mater comes from the Latin for “tender mother,” suggesting the thin membrane is a gentle covering for the brain. The pia extends into every convolution of the CNS, lining the inside of the sulci in the cerebral and cerebellar cortices. At the end of the spinal cord, a thin filament extends from the inferior end of CNS at the upper lumbar region of the vertebral column to the sacral end of the vertebral column. Because the spinal cord does not extend through the lower lumbar region of the vertebral column, a needle can be inserted through the dura and arachnoid layers to withdraw CSF. This procedure is called a lumbar puncture and avoids the risk of damaging the central tissue of the spinal cord. Blood vessels that are nourishing the central nervous tissue are between the pia mater and the nervous tissue.
The Ventricular System
Cerebrospinal fluid (CSF) circulates throughout and around the CNS. In other tissues, water and small molecules are filtered through capillaries as the major contributor to the interstitial fluid. In the brain, CSF is produced in special structures to perfuse through the nervous tissue of the CNS and is continuous with the interstitial fluid. Specifically, CSF circulates to remove metabolic wastes from the interstitial fluids of nervous tissues and return them to the blood stream. The ventricles are the open spaces within the brain where CSF circulates. In some of these spaces, CSF is produced by filtering of the blood that is performed by a specialized membrane known as a choroid plexus. The CSF circulates through all of the ventricles to eventually emerge into the subarachnoid space where it will be reabsorbed into the blood.
The Ventricles
There are four ventricles within the brain, all of which developed from the original hollow space within the neural tube, the central canal. The first two are named the lateral ventricles and are deep within the cerebrum. These ventricles are connected to the third ventricle by two openings called the interventricular foramina. The third ventricle is the space between the left and right sides of the diencephalon, which opens into the cerebral aqueduct that passes through the midbrain. The aqueduct opens into the fourth ventricle, which is the space between the cerebellum and the pons and upper medulla.
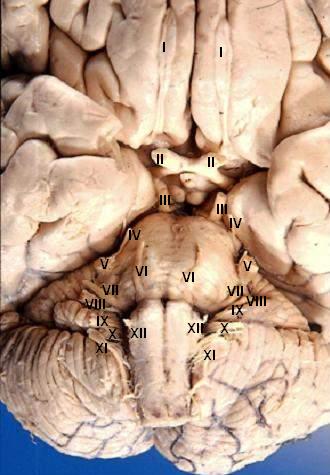
Cranial Nerves
Cranial nerves are the nerves that emerge directly from the brain (including the brainstem), in contrast to spinal nerves (which emerge from segments of the spinal cord). Ten of the cranial nerves originate in the brainstem. Cranial nerves relay information between the brain and parts of the body, primarily to and from regions of the head and neck.
Spinal nerves emerge sequentially from the spinal cord with the spinal nerve closest to the head (C1) emerging in the space above the first cervical vertebra. The cranial nerves, however, emerge from the central nervous system above this level. Each cranial nerve is paired and is present on both sides. Depending on definition in humans there are twelve or thirteen cranial nerves pairs, which are assigned Roman numerals I–XII, sometimes also including cranial nerve zero. The numbering of the cranial nerves is based on the order in which they emerge from the brain, front to back (brainstem).
The, olfactory nerves (I) and optic nerves (II) emerge from the cerebrum or forebrain, and the remaining ten pairs arise from the brainstem, which is the lower part of the brain.
The cranial nerves are considered components of the peripheral nervous system (PNS), although on a structural level the olfactory (I), optic (II), and trigeminal (V) nerves are more accurately considered part of the central nervous system (CNS).
Humans are considered to have twelve pairs of cranial nerves (I–XII). They are: the olfactory nerve (I), the optic nerve (II), oculomotor nerve (III), trochlear nerve (IV), trigeminal nerve (V), abducens nerve (VI), facial nerve (VII), vestibulocochlear nerve (VIII), glossopharyngeal nerve (IX), vagus nerve (X), accessory nerve (XI), and hypoglossal nerve (XII).
The Spinal Cord & Spinal Nerves
Objectives
- Recognize and describe the major surface features of the spinal cord & minges.
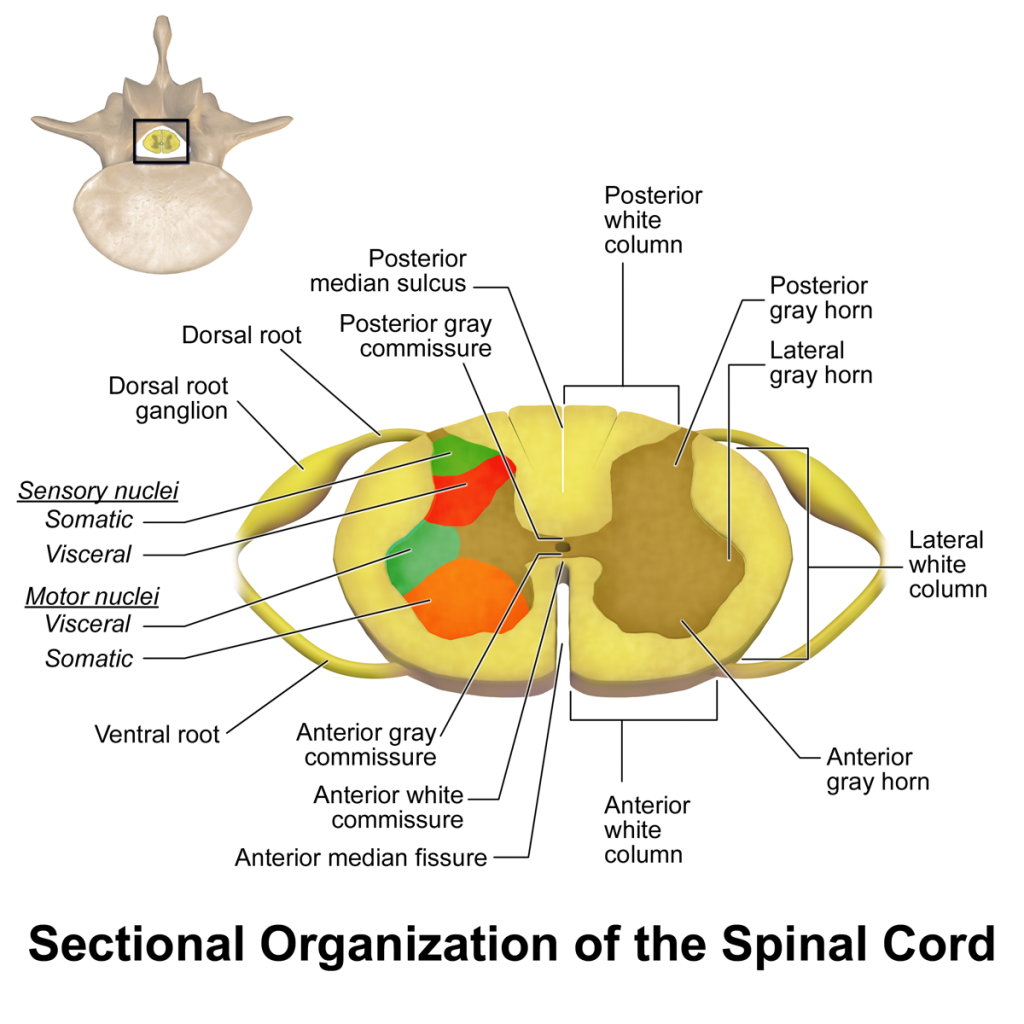
- Recognize and describe the sectional anatomy of the spinal cord.
- Recognize and describe the organization of spinal nerves.
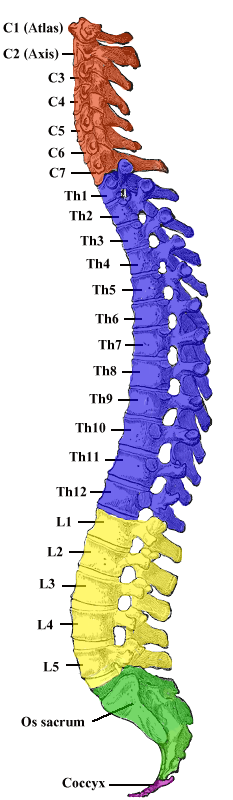
The Spinal Cord
The spinal cord is a long, thin, tubular structure made up of nervous tissue, which extends from the medulla oblongata in the brainstem to the lumbar region of the vertebral column. It encloses the central canal of the spinal cord, which contains cerebrospinal fluid. The brain and spinal cord together make up the central nervous system (CNS). In humans, the spinal cord begins at the occipital bone, passing through the foramen magnum and entering the spinal canal at the beginning of the cervical vertebrae. The spinal cord extends down to between the first and second lumbar vertebrae, where it ends. The enclosing bony vertebral column protects the relatively shorter spinal cord. It is around 45 cm (18 in) in men and around 43 cm (17 in) long in women. The diameter of the spinal cord ranges from 13 mm (1⁄2 in) in the cervical and lumbar regions to 6.4 mm (1⁄4 in) in the thoracic area.
The spinal cord functions primarily in the transmission of nerve signals from the motor cortex to the body, and from the afferent fibers of the sensory neurons to the sensory cortex. It is also a center for coordinating many reflexes and contains reflex arcs that can independently control reflexes. It is also the location of groups of spinal interneurons that make up the neural circuits known as central pattern generators. These circuits are responsible for controlling motor instructions for rhythmic movements such as walking.
Structure
The spinal cord is the main pathway for information connecting the brain and peripheral nervous system. Much shorter than its protecting spinal column, the human spinal cord originates in the brainstem, passes through the foramen magnum, and continues through to the conus medullaris near the second lumbar vertebra before terminating in a fibrous extension known as the filum terminale.
It is about 45 cm (18 in) long in men and around 43 cm (17 in) in women, ovoid-shaped, and is enlarged in the cervical and lumbar regions. The cervical enlargement, stretching from the C5 to T1 vertebrae, is where sensory input comes from and motor output goes to the arms and trunk. The lumbar enlargement, located between L1 and S3, handles sensory input and motor output coming from and going to the legs.
The spinal cord is continuous with the caudal portion of the medulla, running from the base of the skull to the body of the first lumbar vertebra. It does not run the full length of the vertebral column in adults. It is made of 31 segments from which branch one pair of sensory nerve roots and one pair of motor nerve roots. The nerve roots then merge into bilaterally symmetrical pairs of spinal nerves. The peripheral nervous system is made up of these spinal roots, nerves, and ganglia.
The dorsal roots are afferent fascicles, receiving sensory information from the skin, muscles, and visceral organs to be relayed to the brain. The roots terminate in dorsal root ganglia, which are composed of the cell bodies of the corresponding neurons. Ventral roots consist of efferent fibers that arise from motor neurons whose cell bodies are found in the ventral (or anterior) gray horns of the spinal cord.
The spinal cord (and brain) are protected by three layers of tissue or membranes called meninges, that surround the canal. The dura mater is the outermost layer, and it forms a tough protective coating. Between the dura mater and the surrounding bone of the vertebrae is a space called the epidural space. The epidural space is filled with adipose tissue, and it contains a network of blood vessels. The arachnoid mater, the middle protective layer, is named for its open, spiderweb-like appearance. The space between the arachnoid and the underlying pia mater is called the subarachnoid space. The subarachnoid space contains cerebrospinal fluid (CSF), which can be sampled with a lumbar puncture, or “spinal tap” procedure. The delicate pia mater, the innermost protective layer, is tightly associated with the surface of the spinal cord. The cord is stabilized within the dura mater by the connecting denticulate ligaments, which extend from the enveloping pia mater laterally between the dorsal and ventral roots. The dural sac ends at the vertebral level of the second sacral vertebra.
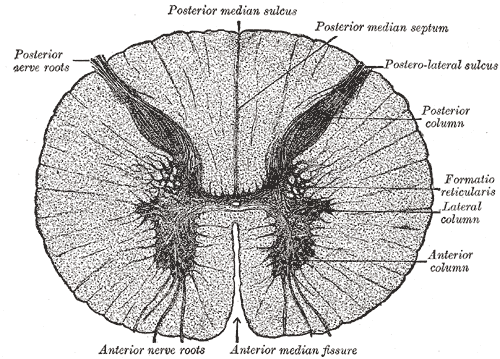
In cross-section, the peripheral region of the cord contains neuronal white matter tracts containing sensory and motor axons. Internal to this peripheral region is the grey matter, which contains the nerve cell bodies arranged in the three grey columns that give the region its butterfly-shape. This central region surrounds the central canal, which is an extension of the fourth ventricle and contains cerebrospinal fluid.
The spinal cord is elliptical in cross section, being compressed dorsolaterally. Two prominent grooves, or sulci, run along its length. The posterior median sulcus is the groove in the dorsal side, and the anterior median fissure is the groove in the ventral side.
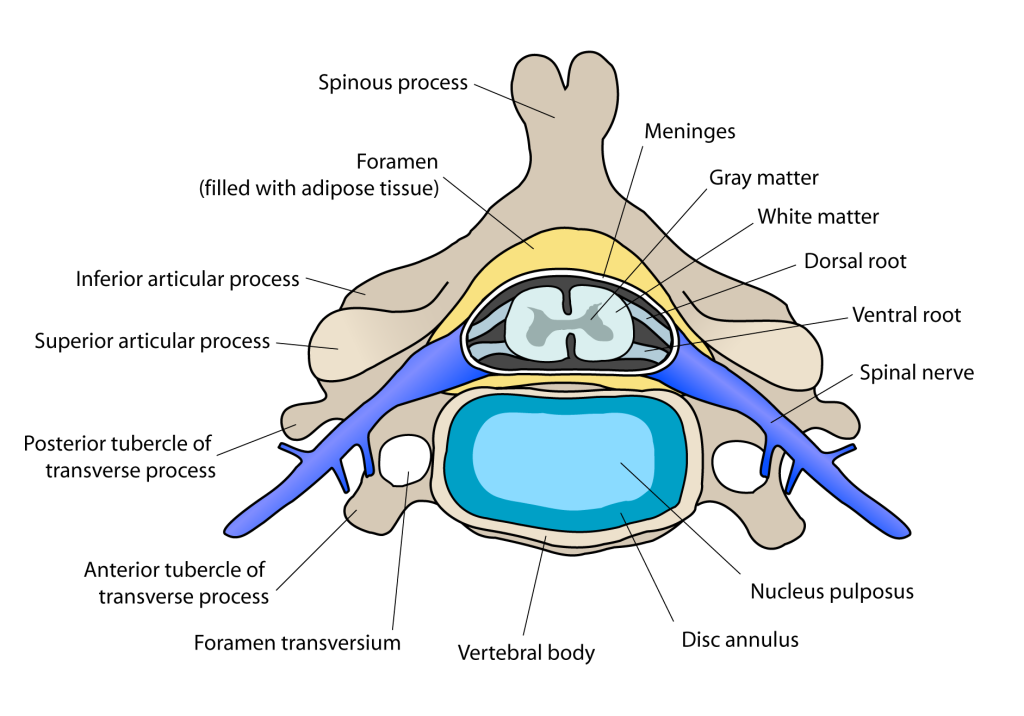
Meninges
The meninges are the three membranes that envelop the brain and spinal cord. In mammals, the meninges are the dura mater, the arachnoid mater, and the pia mater. Cerebrospinal fluid is located in the subarachnoid space between the arachnoid mater and the pia mater. The primary function of the meninges is to protect the central nervous system.
Dura mater
The dura mater is a thick, durable membrane, closest to the skull and vertebrae. The dura mater, the outermost part, is a loosely arranged, fibroelastic layer of cells, characterized by multiple interdigitating cell processes, no extracellular collagen, and significant extracellular spaces. The middle region is a mostly fibrous portion. It consists of two layers: the endosteal layer, which lies closest to the calvaria (skullcap), and the inner meningeal layer, which lies closer to the brain. It contains larger blood vessels that split into the capillaries in the pia mater. It is composed of dense fibrous tissue, and its inner surface is covered by flattened cells like those present on the surfaces of the pia mater and arachnoid mater. The dura mater is a sac that envelops the arachnoid mater and surrounds and supports the large dural sinuses carrying blood from the brain toward the heart.
The dura has four areas of infolding:
- Falx cerebri, the largest, sickle-shaped, separates the cerebral hemispheres. Starts from the frontal crest of frontal bone and the crista galli running to the internal occipital protuberance.
- Tentorium cerebelli, the second largest, crescent-shaped; separates the occipital lobes from cerebellum. The falx cerebri attaches to it giving a tentlike appearance.
- Falx cerebelli, vertical infolding; lies inferior to the tentorium cerebelli, separating the cerebellar hemispheres.
- Diaphragma sellae, smallest infolding; covers the pituitary gland and sella turcica.
Arachnoid Mater
The middle element of the meninges is the arachnoid mater, so named because of its spider web-like appearance. It cushions the central nervous system. This thin, transparent membrane is composed of fibrous tissue and, like the pia mater, is covered by flat cells also thought to be impermeable to fluid.
The shape of the arachnoid does not follow the convolutions of the surface of the brain and so looks like a loosely fitting sac. In particular, in the region of the brain a large number of fine filaments called arachnoid trabeculae pass from the arachnoid through the subarachnoid space to blend with the tissue of the pia mater. The arachnoid is composed of an outermost portion (arachnoid barrier cell layer) with tightly packed cells and no extracellular collagen; that is why it is considered to represent an effective morphological and physiological meningeal barrier between the cerebrospinal fluid and subarachnoid space and the blood circulation in the dura.
The arachnoid barrier layer is characterized by a distinct continuous basal lamina on its inner surface toward the innermost collagenous portion of the arachnoid reticular layer
Pia Mater
The pia mater is a very delicate membrane. It is the meningeal envelope that firmly adheres to the surface of the brain and spinal cord, following all of the brain’s contours (the gyri and sulci). It is a very thin membrane composed of fibrous tissue covered on its outer surface by a sheet of flat cells thought to be impermeable to fluid. The pia mater is pierced by blood vessels to the brain and spinal cord, and its capillaries nourish the brain.
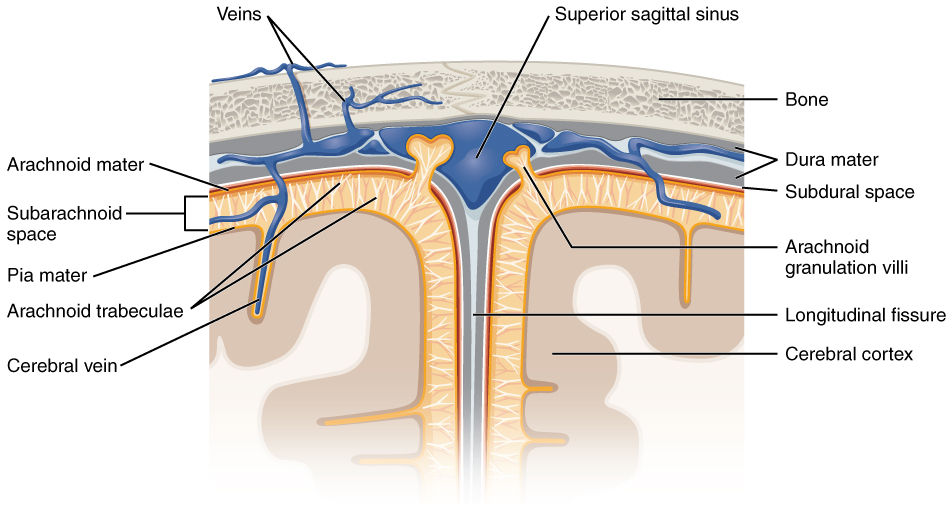
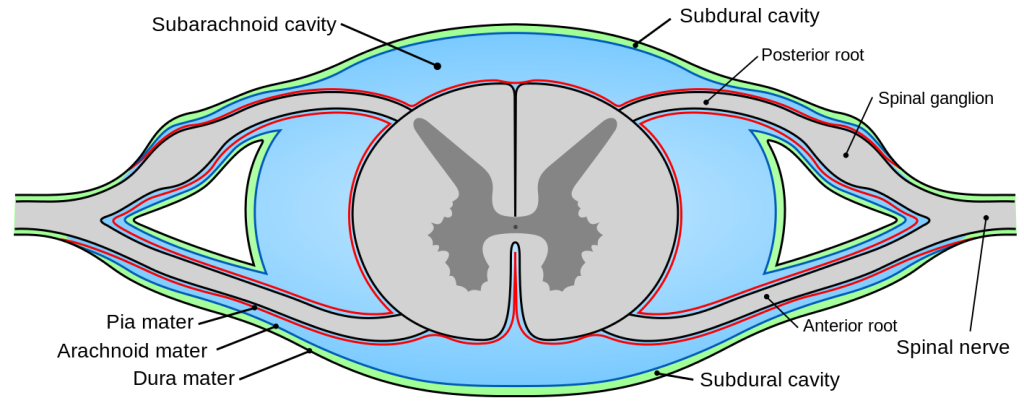
Subarachnoid Space
The subarachnoid space is the space that normally exists between the arachnoid and the pia mater, which is filled with cerebrospinal fluid, and continues down the spinal cord. Spaces are formed from openings at different points along the subarachnoid space; these are the subarachnoid cisterns, which are filled with cerebrospinal fluid.
The dura mater is attached to the skull, whereas in the spinal cord, the dura mater is separated from the vertebrae by a space called the epidural space, which contains fat and blood vessels. The arachnoid is attached to the dura mater, while the pia mater is attached to the central nervous system tissue. When the dura mater and the arachnoid separate through injury or illness, the space between them is the subdural space. There is a subpial space underneath the pia mater that separates it from the glia limitans.
Spinal Cord Segments
The human spinal cord is divided into segments where pairs of spinal nerves (mixed; sensory and motor) form. Six to eight motor nerve rootlets branch out of right and left ventro lateral sulci in a very orderly manner. Nerve rootlets combine to form nerve roots. Likewise, sensory nerve rootlets form off right and left dorsal lateral sulci and form sensory nerve roots. The ventral (motor) and dorsal (sensory) roots combine to form spinal nerves (mixed; motor and sensory), one on each side of the spinal cord. Spinal nerves, with the exception of C1 and C2, form inside the intervertebral foramen (IVF). These rootlets form the demarcation between the central and peripheral nervous systems.
The grey column, (as three regions of grey columns) in the center of the cord, is shaped like a butterfly and consists of cell bodies of interneurons, motor neurons, neuroglia cells and unmyelinated axons. The anterior and posterior grey column present as projections of the grey matter and are also known as the horns of the spinal cord. Together, the grey columns and the gray commissure form the “grey H.”
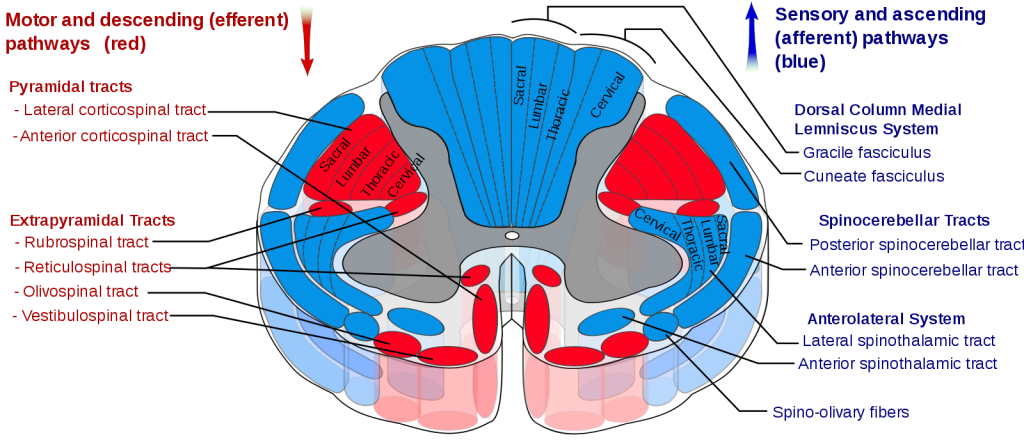
The white matter is located outside of the grey matter and consists almost totally of myelinated motor and sensory axons. “Columns” of white matter carry information either up or down the spinal cord.
The spinal cord proper terminates in a region called the conus medullaris, while the pia mater continues as an extension called the filum terminale, which anchors the spinal cord to the coccyx. The cauda equina (“horse’s tail”) is a collection of nerves inferior to the conus medullaris that continue to travel through the vertebral column to the coccyx. The cauda equina forms because the spinal cord stops growing in length at about age four, even though the vertebral column continues to lengthen until adulthood. This results in sacral spinal nerves originating in the upper lumbar region.
Within the CNS, nerve cell bodies are generally organized into functional clusters, called nuclei. Axons within the CNS are grouped into tracts.
There are 31 spinal cord nerve segments in a human spinal cord:
- 8 cervical segments forming 8 pairs of cervical nerves (C1 spinal nerves exit the spinal column between the foramen magnum and the C1 vertebra; C2 nerves exit between the posterior arch of the C1 vertebra and the lamina of C2; C3–C8 spinal nerves pass through the IVF above their corresponding cervical vertebrae, with the exception of the C8 pair which exit between the C7 and T1 vertebrae)
- 12 thoracic segments forming 12 pairs of thoracic nerves
- 5 lumbar segments forming 5 pairs of lumbar nerves
- 5 sacral segments forming 5 pairs of sacral nerves
- 1 coccygeal segment
Somatosensory Organization
Somatosensory organization is divided into the dorsal column-medial lemniscus tract (the touch/proprioception/vibration sensory pathway) and the anterolateral system, or ALS (the pain/temperature sensory pathway). Both sensory pathways use three different neurons to get information from sensory receptors at the periphery to the cerebral cortex. These neurons are designated primary, secondary and tertiary sensory neurons. In both pathways, primary sensory neuron cell bodies are found in the dorsal root ganglia, and their central axons project into the spinal cord.
In the dorsal column-medial leminiscus tract, a primary neuron’s axon enters the spinal cord and then enters the dorsal column. If the primary axon enters below spinal level T6, the axon travels in the fasciculus gracilis, the medial part of the column. If the axon enters above level T6, then it travels in the fasciculus cuneatus, which is lateral to the fasciculus gracilis. Either way, the primary axon ascends to the lower medulla, where it leaves its fasciculus and synapses with a secondary neuron in one of the dorsal column nuclei: either the nucleus gracilis or the nucleus cuneatus, depending on the pathway it took. At this point, the secondary axon leaves its nucleus and passes anteriorly and medially. The collection of secondary axons that do this are known as internal arcuate fibers. The internal arcuate fibers decussate and continue ascending as the contralateral medial lemniscus. Secondary axons from the medial lemniscus finally terminate in the ventral posterolateral nucleus (VPLN) of the thalamus, where they synapse with tertiary neurons. From there, tertiary neurons ascend via the posterior limb of the internal capsule and end in the primary sensory cortex.
The proprioception of the lower limbs differs from the upper limbs and upper trunk. There is a four-neuron pathway for lower limb proprioception. This pathway initially follows the dorsal spino-cerebellar pathway. It is arranged as follows: proprioceptive receptors of lower limb → peripheral process → dorsal root ganglion → central process → Clarke’s column → 2nd order neuron → medulla oblongata (Caudate nucleus) → 3rd order neuron → VPLN of thalamus → 4th order neuron → posterior limb of internal capsule → corona radiata → sensory area of cerebrum.
The anterolateral system works somewhat differently. Its primary neurons axons enter the spinal cord and then ascend one to two levels before synapsing in the substantia gelatinosa. The tract that ascends before synapsing is known as Lissauer’s tract. After synapsing, secondary axons decussate and ascend in the anterior lateral portion of the spinal cord as the spinothalamic tract. This tract ascends all the way to the VPLN, where it synapses on tertiary neurons. Tertiary neuronal axons then travel to the primary sensory cortex via the posterior limb of the internal capsule.
Some of the “pain fibers” in the ALS deviate from their pathway towards the VPLN. In one such deviation, axons travel towards the reticular formation in the midbrain. The reticular formation then projects to a number of places including the hippocampus (to create memories about the pain), the centromedian nucleus (to cause diffuse, non-specific pain) and various parts of the cortex. Additionally, some ALS axons project to the periaqueductal gray in the pons, and the axons forming the periaqueductal gray then project to the nucleus raphes magnus, which projects back down to where the pain signal is coming from and inhibits it. This helps control the sensation of pain to some degree.
Motor Organization
The corticospinal tract serves as the motor pathway for upper motor neuronal signals coming from the cerebral cortex and from primitive brainstem motor nuclei.
Cortical upper motor neurons originate from Brodmann areas 1, 2, 3, 4, and 6 and then descend in the posterior limb of the internal capsule, through the crus cerebri, down through the pons, and to the medullary pyramids, where about 90% of the axons cross to the contralateral side at the decussation of the pyramids. They then descend as the lateral corticospinal tract. These axons synapse with lower motor neurons in the ventral horns of all levels of the spinal cord. The remaining 10% of axons descend on the ipsilateral side as the ventral corticospinal tract. These axons also synapse with lower motor neurons in the ventral horns. Most of them will cross to the contralateral side of the cord (via the anterior white commissure) right before synapsing.
The midbrain nuclei include four motor tracts that send upper motor neuronal axons down the spinal cord to lower motor neurons. These are the rubrospinal tract, the vestibulospinal tract, the tectospinal tract and the reticulospinal tract. The rubrospinal tract descends with the lateral corticospinal tract, and the remaining three descend with the anterior corticospinal tract.
The function of lower motor neurons can be divided into two different groups: the lateral corticospinal tract and the anterior corticospinal tract. The lateral tract contains upper motor neuronal axons which synapse on dorsal lateral (DL) lower motor neurons. The DL neurons are involved in distal limb control. Therefore, these DL neurons are found specifically only in the cervical and lumbosacral enlargements within the spinal cord. There is no decussation in the lateral corticospinal tract after the decussation at the medullary pyramids.
The anterior corticospinal tract descends ipsilaterally in the anterior column, where the axons emerge and either synapse on lower ventromedial (VM) motor neurons in the ventral horn ipsilateral or decussate at the anterior white commissure where they synapse on VM lower motor neurons contralaterally . The tectospinal, vestibulospinal and reticulospinal descend ipsilaterally in the anterior column but do not synapse across the anterior white commissure. Rather, they only synapse on VM lower motor neurons ipsilateral. The VM lower motor neurons control the large, postural muscles of the axial skeleton. These lower motor neurons, unlike those of the DL, are located in the ventral horn all the way throughout the spinal cord.
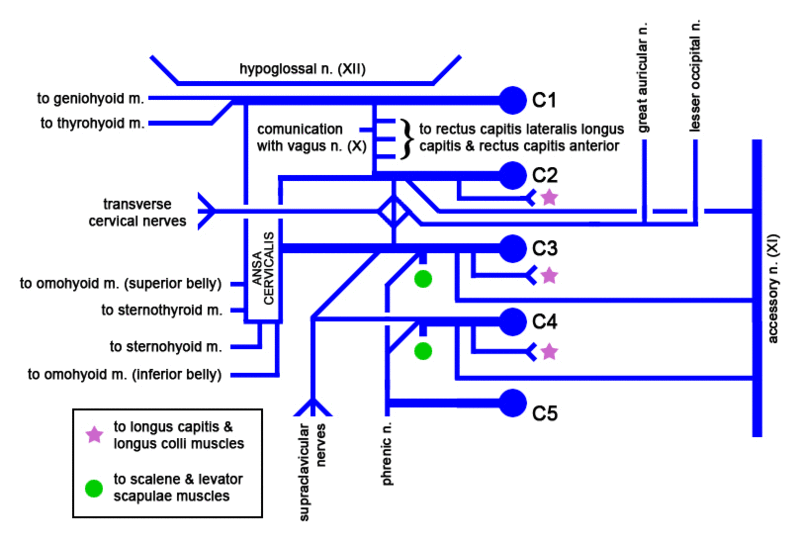
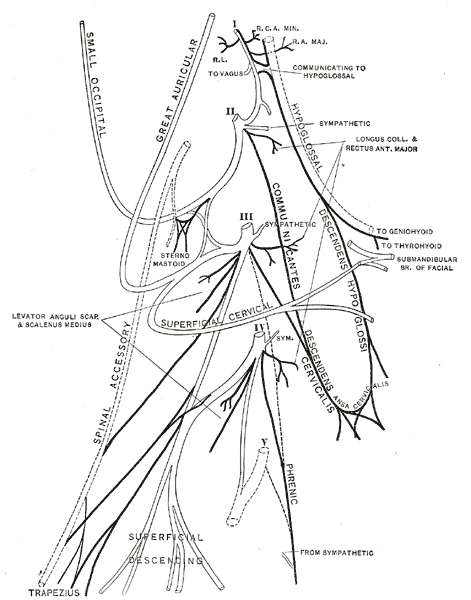
Cervical Plexus
The cervical plexus is a plexus of the anterior rami of the first four cervical spinal nerves which arise from C1 to C4 cervical segment in the neck. They are located laterally to the transverse processes between prevertebral muscles from the medial side and vertebral (m. scalenus, m. levator scapulae, m. splenius cervicis) from lateral side. There is anastomosis with accessory nerve, hypoglossal nerve and sympathetic trunk.
It is located in the neck, deep to sternocleidomastoid m. Nerves formed from the cervical plexus innervate the back of the head, as well as some neck muscles. The branches of the cervical plexus emerge from the posterior triangle at the nerve point, a point which lies midway on the posterior border of the sternocleidomastoid. Also from the posterior ramus of C2 greater occipital nerve arises
The cervical plexus has two types of branches: cutaneous and muscular.
Cutaneous (4 branches):
- Lesser occipital – innervates the skin and the scalp posterosuperior to the auricle (C2)
- Great auricular nerve – innervates skin near concha auricle (outer ear) and external acoustic meatus (ear canal) (C2&C3)
- Transverse cervical nerve – innervates anterior region of neck (C2&C3)
- Supraclavicular nerves – innervate the skin above and below the clavicle (C3,C4) [1]
Muscular
- Ansa cervicalis (This is a loop formed from C1-C3 which supplies the four infrahyoid aka strap muscles), etc. (thyrohyoid (C1 only), sternothyroid, sternohyoid, omohyoid)
- Phrenic (C3-C5 (primarily C4))-innervates diaphragm and the pericardium
- Segmental branches (C1-C4)- innervates anterior and middle scalenes
- Additionally, there are two branches formed by the posterior roots of spinal nerves:
- Preauricular nerve (from the posterior roots of C2–C3)[2][3]
- Postauricular nerve (from the posterior roots of C3–C4)[3]
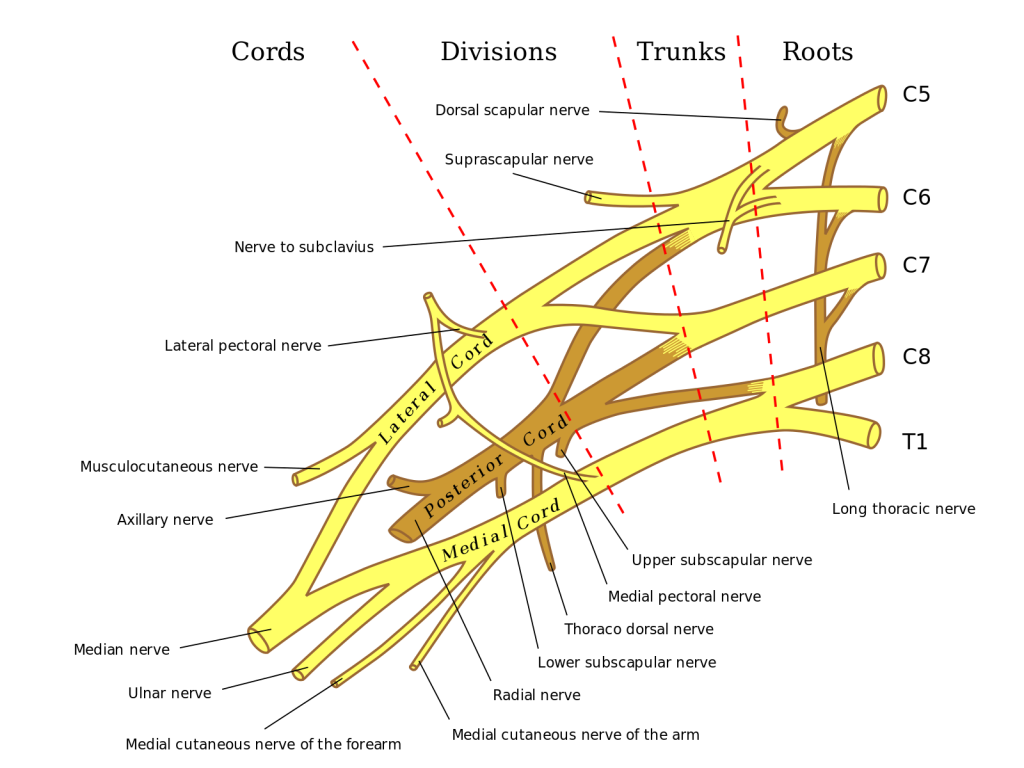
Brachial Plexus
The brachial plexus is a network (plexus) of nerves (formed by the ventral ramus of the lower four cervical nerves and first thoracic nerve (C5, C6, C7, C8, and T1). This plexus extends from the spinal cord, through the cervicoaxillary canal in the neck, over the first rib, and into the armpit. It supplies afferent and efferent nerve fibers to the chest, shoulder, arm and hand.
The brachial plexus is divided into five roots, three trunks, six divisions (three anterior and three posterior), three cords, and five branches. There are five “terminal” branches and numerous other “pre-terminal” or “collateral” branches, such as the subscapular nerve, the thoracodorsal nerve, and the long thoracic nerve,[1] that leave the plexus at various points along its length. A common structure used to identify part of the brachial plexus in cadaver dissections is the M or W shape made by the musculocutaneous nerve, lateral cord, median nerve, medial cord, and ulnar nerve.
Roots
The five roots are the five anterior rami of the spinal nerves, after they have given off their segmental supply to the muscles of the neck. The brachial plexus emerges at five different levels; C5, C6, C7, C8, and T1. C5 and C6 merge to establish the upper trunk, C7 continuously forms the middle trunk, and C8 and T1 merge to establish the lower trunk. Prefixed or postfixed formations in some cases involve C4 or T2, respectively. The dorsal scapular nerve comes from the superior trunk and innervates the rhomboid muscles which retract the scapula. The subclavian nerve originates in both C5 and C6 and innervates the subclavius, a muscle that involves lifting the first ribs during respiration. The long thoracic nerve arises from C5, C6, and C7. This nerve innervates the serratus anterior, which draws the scapula laterally and is the prime mover in all forward-reaching and pushing actions.
Trunks
These roots merge to form the trunks:
Divisions
Each trunk then splits in two, to form six divisions:
- anterior divisions of the upper, middle, and lower trunks
- posterior divisions of the upper, middle, and lower trunks
- when observing the body in the anatomical position, the anterior divisions are superficial to the posterior divisions
Cords
These six divisions regroup to become the three cords or large fiber bundles. The cords are named by their position with respect to the axillary artery.
- The posterior cord is formed from the three posterior divisions of the trunks (C5-C8, T1)
- The lateral cord is formed from the anterior divisions of the upper and middle trunks (C5-C7)
- The medial cord is simply a continuation of the anterior division of the lower trunk (C8, T1)
Laboratory Activity
Label the main part of the Central Nervous System
Label the hemispheres of the brain and the longitudinal fissure.
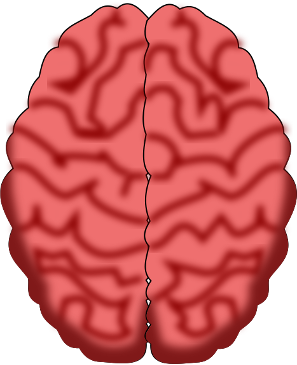
The brain
Label the main regions of the brain.
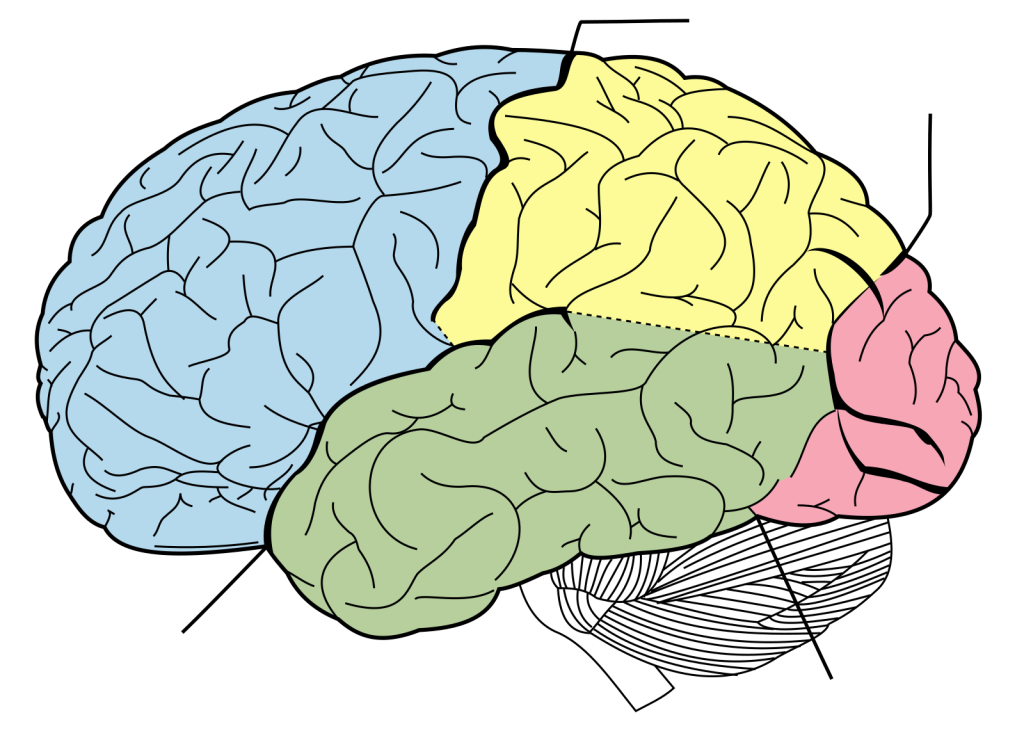
The brain
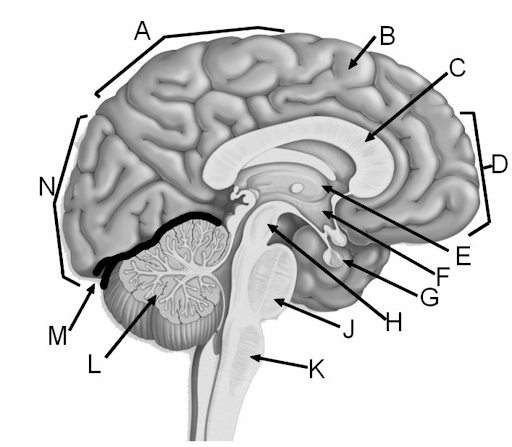
Sagittal section of brain
| Letter | Structure |
| A | |
| B | |
| C | |
| D | |
| E | |
| F | |
| G | |
| H | |
| I | |
| J | |
| K | |
| L | |
| M |
Label the 12 pairs of Cranial Nerves
| # | Structure |
| 1 | |
| 2 | |
| 3 | |
| 4 | |
| 5 | |
| 6 | |
| 7 | |
| 8 |
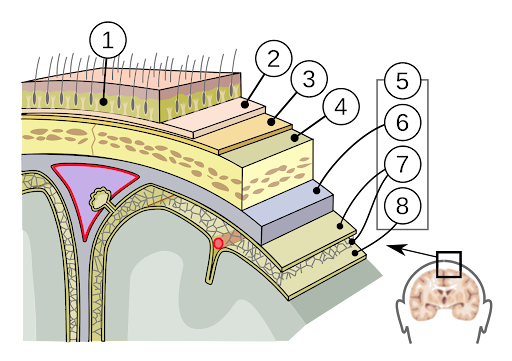
Label the parts of the human spinal cord and the spinal nerve roots
Word bank:
central canal
posterior median sulcus
gray matter
white matter
dorsal root (left)
dorsal root ganglion (right)
ventral root
fascicles
anterior spinal artery
arachnoid mater
dura mater
Label the parts of the human spinal cord and the spinal nerve roots
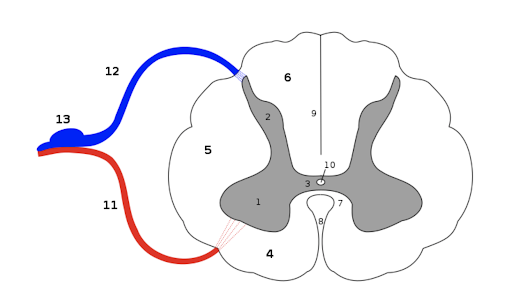
Transverse section of spinal cord
| # | Structure |
| 1 | |
| 2 | |
| 3 | |
| 4 | |
| 5 | |
| 6 | |
| 7 | |
| 8 | |
| 9 | |
| 10 | |
| 11 | |
| 12 | |
| 13 |
Media Attributions
- The Cerebrum © Wikipedia is licensed under a CC BY (Attribution) license
- Lobes of the Cerebral Cortex © Jonathan Akin via. Human Anatomy and Physiology is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Brodmann’s Areas of the Cerebral Cortex © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Types of Cortical Areas © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Head and neck vessels © OpenStax College is licensed under a CC BY-SA (Attribution ShareAlike) license
- Dural Sinuses and Veins © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Meningeal layers © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Cerebrospinal Fluid Circulation © By OpenStax - https://cnx.org/contents/FPtK1zmh@8.25:fEI3C8Ot@10/Preface, CC BY 4.0, https://commons.wikimedia.org/w/index.php?curid=30147960 is licensed under a CC BY-SA (Attribution ShareAlike) license
- Brain normal inferior view © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Brain anterior inferior view © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Brain stem sagittal © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- The spinal cord © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Vertebral column © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Cervical vertebra © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Posterior median sulcus © Wikipedia is licensed under a Public Domain license
- Spinal Cord Sectional Anatomy © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Meninges © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Section of the medulla spinalis © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Spinal cord tracts © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Cervical plexus © Wikipedia
- Plan of the cervical plexus © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Brachial plexus © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Private: Central nervous system © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- The brain © LibreTexts is licensed under a CC BY-SA (Attribution ShareAlike) license
- Label brain regions © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license
- Label brain © Quizlet is licensed under a CC BY-SA (Attribution ShareAlike) license
- Label skull brain © By Patrick J. Lynch, medical illustrator - Patrick J. Lynch, medical illustrator, CC BY 2.5, https://commons.wikimedia.org/w/index.php?curid=1496715 is licensed under a CC BY-SA (Attribution ShareAlike) license
- Label Meninges © CleanPNG Brain Clippart is licensed under a CC BY-SA (Attribution ShareAlike) license
- Label spinal cord © By Tomáš Kebert & umimeto.org - Own work, CC BY-SA 4.0, https://commons.wikimedia.org/w/index.php?curid=94075350 is licensed under a CC BY-SA (Attribution ShareAlike) license
- Label Medulla spinalis © Wikipedia is licensed under a CC BY-SA (Attribution ShareAlike) license