Chapter 11: Biopsychology of Psychological Disorders
11.4: Anxiety
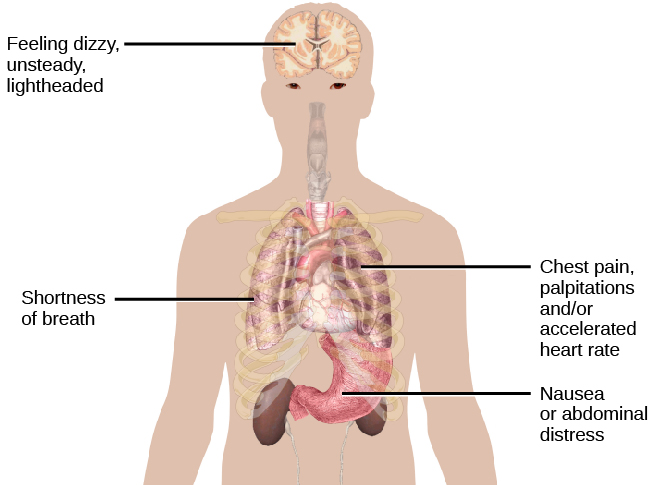
What is anxiety? Most of us feel some anxiety almost every day of our lives. Maybe you have an important upcoming test, presentation, big game, or date. Anxiety can be defined as a negative mood state that is accompanied by bodily symptoms such as increased heart rate, muscle tension, a sense of unease, and apprehension about the future (APA, 2013; Barlow, 2002) (Figure 4).
Anxiety disorders are characterized by excessive and persistent fear and anxiety, and by related disturbances in behavior (APA, 2013). Although anxiety is universally experienced, anxiety disorders cause considerable distress. As a group, anxiety disorders are common: approximately 25–30% of the U.S. population meets the criteria for at least one anxiety disorder during their lifetime (Kessler et al., 2005). Also, anxiety disorders are much more common in women than they are in men; within a 12-month period, around 23% of women and 14% of men will experience at least one anxiety disorder (National Comorbidity Survey, 2007). Anxiety disorders are the most frequently occurring class of mental disorders and are often comorbid with each other and with other mental disorders (Kessler et al., 2009).[1]
Neural mechanisms underlying anxiety disorders
Anxiety disorders are associated with genetic factors and abnormalities in brain circuits that regulate and process emotion. Family and twin studies indicate that anxiety disorders have a moderate genetic heritability (~30-40%; making it less heritable than schizophrenia or bipolar disorder) (Hettema et al., 2001). More than 200 genes are associated with anxiety disorders, and distinct gene clusters exist for different anxiety subtypes such as generalized anxiety disorder, social anxiety disorder, and panic disorder. The identified genes are expressed in brain regions (e.g., the basal ganglia, hippocampus, and amygdala) that are linked to anxiety and emotion processing (Karunakaran & Amemori, 2023).
The brain circuits underlying anxiety involve bottom-up signals from the amygdala that indicate presence of potentially threatening stimuli, and top-down control mechanisms from the prefrontal cortex that signal the emotional salience of stimuli (Nuss, 2015). The amygdala is involved in triggering panic attacks through its central nucleus, which connects with brain structures, particularly in the brainstem, that control autonomic functions such as respiration and heart rate. Animal studies have shown that electrically or pharmacologically stimulating the amygdala’s central nucleus produces behaviors associated with panic (Herdade et al., 2006). People with an anxiety disorder show hyperactive amygdala response to stimuli (Etkin & Wager, 2007); these bottom-up signals from the amygdala might be over-indicating the presence of potentially threatening stimuli. “Top-down” control originating from prefrontal areas can regulate emotion by inhibiting amygdala output; however, neuroimaging studies show that people with anxiety disorders have reduced activation in prefrontal circuits (Etkin, 2010), and interestingly they required higher levels of prefrontal activation to successfully reduce negative emotions (Nuss, 2015).
Research examining the role of neurotransmitters in anxiety-related circuits has focused largely on GABA, the primary inhibitory neurotransmitter in the brain that reduces neuronal excitability. Insufficient GABAergic inhibition of neurons might drive the amygdala hyperactivity seen in anxiety disorders. Therefore GABA receptors are a primary target for anti-anxiety medication. In animal studies, injections of GABA agonists (activators) into the amygdala decreased measures of fear and anxiety (Sanders & Shekhar, 1995). GABA receptors can be modulated by a class of drugs called benzodiazepines, that include well-known brand names like Valium, Xanax, and Ativan. Benzodiazepines work by binding to the GABAA receptor complex, which increases the total conduction of chloride (Cl-) ions across the cell membrane. The increased concentration of negative chloride ions hyperpolarizes the neuron’s membrane potential, thereby inhibiting it and making it less likely to fire. Through this increased neuronal inhibition, benzodiazepines can reduce anxiety and reduce the amygdala’s response to aversive stimuli (Del-Ben et al., 2012).
Benzodiazepines were the most common pharmacological treatment for anxiety for many decades. But due to their highly addictive properties and lack of long-term effectiveness, benzodiazepines are now recommended only for short-term treatments of anxiety (2-4 weeks). While GABA is an important target for modulating anxiety responses in the amygdala, other neurotransmitters such as serotonin, endocannabinoids, and oxytocin, are also important. Current treatment guidelines for anxiety disorders now recommend antidepressants, including serotonin reuptake inhibitors (SSRIs) or serotonin–noradrenaline reuptake inhibitors (Nuss, 2015).
For non-pharmacological treatments, cognitive behavioral therapy (CBT) is well established, and successful CBT treatment of anxiety disorders has been shown to stop amygdala hyperactivation (Straube et al., 2006). Finally, even placebos have been shown to decrease anxiety; when individuals thought they received an anti-anxiety drug, some showed a lower anxiety response to emotional pictures. Their placebo response was associated with decreased activation in the amygdala, as well as increased activation in a modulatory system including the anterior cingulate and the prefrontal cortex (Petrovic et al., 2005). In sum, irrespective of the technique, anxiety can be reduced by decreasing activation in the amygdala or increasing activation in modulatory or emotion-regulating circuits, and ongoing research seeks to optimize how these networks can be targeted to manage anxiety.
Media Attributions
- Physical manifestations of a panic attack © OpenStax is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- This section contains material adapted from: Barlow, D. H. & Ellard, K. K. (2024). Anxiety and related disorders. In R. Biswas-Diener & E. Diener (Eds.), Noba textbook series: Psychology. Champaign, IL: DEF publishers. Retrieved from http://noba.to/xms3nq2c License: CC BY-NC-SA 4.0 DEED - Spielman, R. M., Jenkins, W. J., & Lovett, M. D. (2020). 15.4 Anxiety Disorders. In Psychology 2e. OpenStax. Access for free at https://openstax.org/books/psychology-2e/pages/15-4-anxiety-disorders License: CC BY 4.0 DEED. ↵
Intense, excessive, and persistent worry and fear about everyday situations. Linked to heightened physical sensations, such as fast heart rate, rapid breathing, sweating, and fatigue
A group of disorders that are characterized by excessive and persistent feelings of intense worry, fear, and dread, as well as physical sensations like increased blood pressure and fast heart rate
Spherical cell group located in the amygdala that is primarily responsible for the bodily reactions associated with fear