Treating cancer: targeting the hallmarks of cancer
If a person is diagnosed with a solid tumor, typically the first goal will be surgical removal of the tumor. This often includes treatment to kill off any remaining cancer cells, including any cells that may have metastasized. Once metastasis has occurred, it can be very difficult, if not impossible, to surgically remove all cancer cells.
It is a challenge to use nonsurgical means to kill off cancer cells. Unlike taking an antibiotic to kill a bacterial infection, cancer cells are part of a patient’s own body. Any drug or treatment that can kill cancer cells will likely also damage healthy tissue. So the goal is to find a drug or treatment that kills cancer cells but leaves healthy tissue alone as much as possible. Sometimes, this therapeutic window is quite small.
Traditionally, oncology treatments have targeted two main characteristics of cancer that make them different from healthy cells: uncontrolled growth and genetic instability.
Most traditional chemotherapies work by exploiting the uncontrolled growth of cancer cells, using various drugs to kill the most rapidly dividing cells in the body. Unfortunately, cancer cells are not the only rapidly dividing cells: hair follicles and the lining of the digestive tract are two examples of other rapidly dividing cell types. Thus, patients being treated with chemotherapies often lose their hair and have digestive challenges as side effects of the drug treatment.
Other chemotherapies as well as radiation exploit the DNA repair defects of cancer cells. Although radiation induces DNA damage and therefore can lead to cancer, tumor cells that lack functional repair mechanisms are especially susceptible to radiation. Essentially, low levels of damage can cause cancer, but high amounts of damage will just kill the cell. Certain chemotherapies also work by causing DNA damage. But again, these therapies also damage healthy cells, just hopefully not as much as the cancer cells.
But in the last twenty years, cancer research has been focused on finding targeted strategies for fighting cancer: ones that are more specific to killing cancer cells but will have little effect on healthy ones.
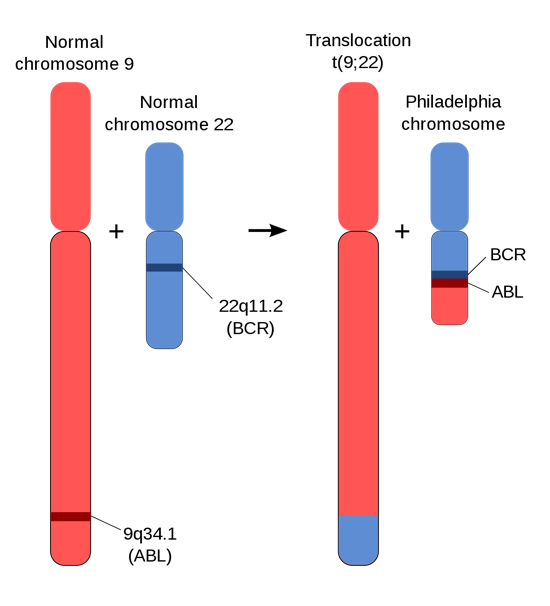
The most successful example to date has been the drug imatinib, which targets an oncogene called BCR-ABL. The BCR-ABL oncogene does not exist in healthy cells. It is a fusion protein created by a translocation common to chronic myelogenous leukemia (CML) and other cancers, as shown in Figure 22. The drug inhibits the BCR-ABL mutation that drives the cancer and blocks cancer cell proliferation, but it has little effect on healthy cells because they do not have the oncogene. With imatinib treatment, life expectancy of CML patients is similar to that of noncancer patients.
Other examples target growth receptors found on the cell surface of cancer cells or exploit the hallmarks of cancer. This includes new therapies that program the immune system to recognize and fight specific types of cancer.
Despite these remarkable advances, we still remain a long way from “a cure” for cancer. Because of the varied mutations that contribute to cancer, each of these innovations only helps a very select population of patients.
Media Attributions
- Figure 22 DNA Repair © By Aryn89 is licensed under a CC BY-SA (Attribution ShareAlike) license

